EXPLORING THE NEXT GENERATION INTENSIVE CARE UNIT OF THE FUTURE
A collaborative co-design studio between the Department of Design and Department of Surgery, The Ohio State University
This was a collaborative co-design studio between the Department of Design and the Department of Surgery, The Ohio State University. The studio was centered on near and long-term needs within the surgical intensive care units at the Arthur G. James Cancer Hospital and the Ohio State University Wexner Medical Center. We had the opportunity to work directly with healthcare professionals and immersed ourselves in their working environments. It was an intriguing hands-on experience in a real-world challenge in an interdisciplinary setting. The end goals for the OSUWMC Department of Surgery included an objective and broad-based assessment of the current ICU experience and the opportunity for the healthcare professions to join the graduate students in the design-led exploration of future scenarios of use.
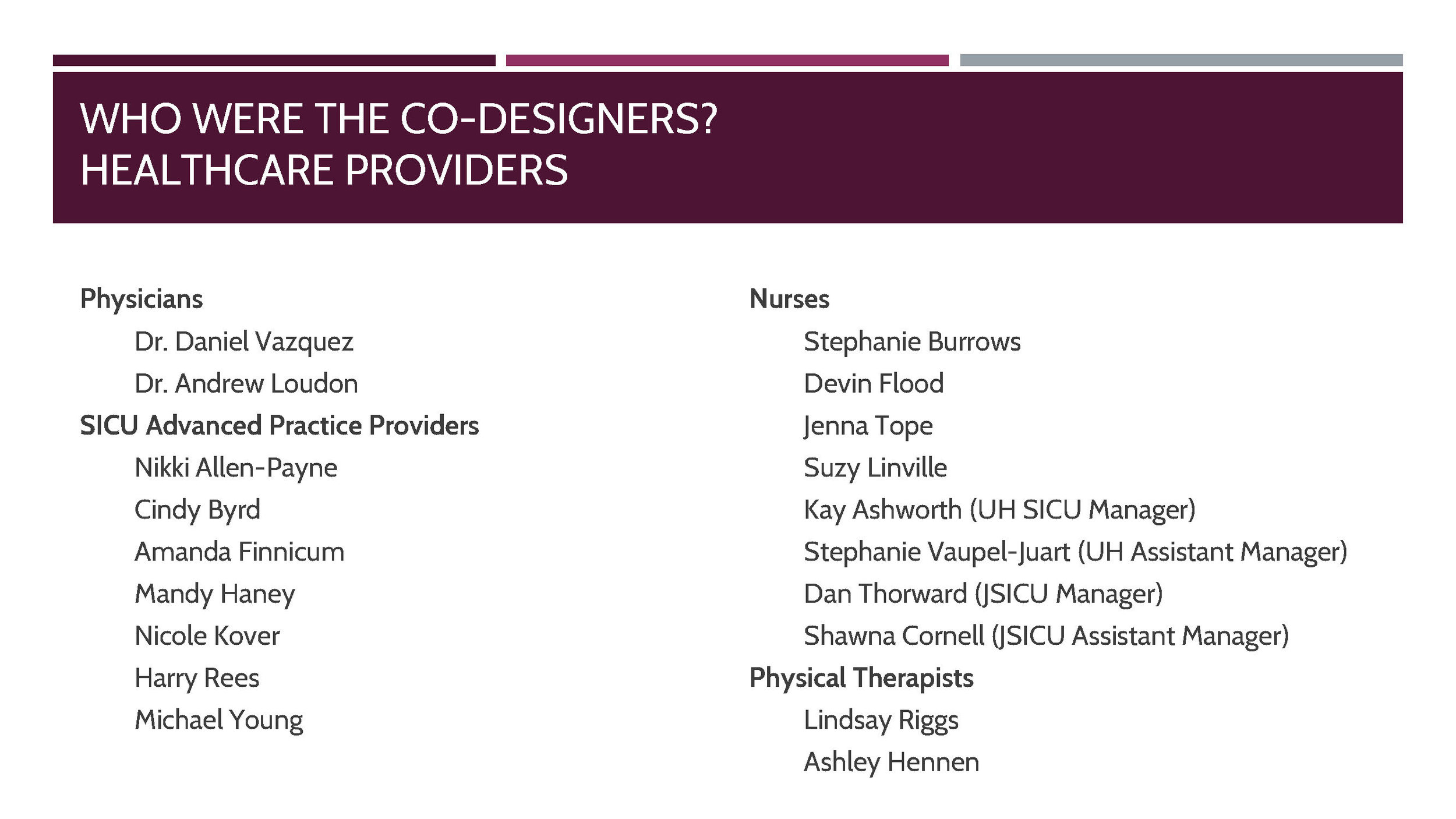
Core Medical Team: Dr. Daniel Vazquez, MD, MSc, FACS – Medical Co-PI for the project, Amanda Haney – Lead Nurse Practitioner, Surgical Intensive Care Unit, and Cindy Byrd – Advanced Practice Manager, Critical Care
Medical Support Structure: Steven Steinberg – Director, Surgical Intensive Care Unit, Dr Timothy Pawlik – Chairman, Surgery Department, Kay Ashworth – Nurse Manager, Surgical Intensive Care Unit, Dan Thorward – Nurse Manager, James Surgical Intensive Care Unit
Phase 1: Immersion
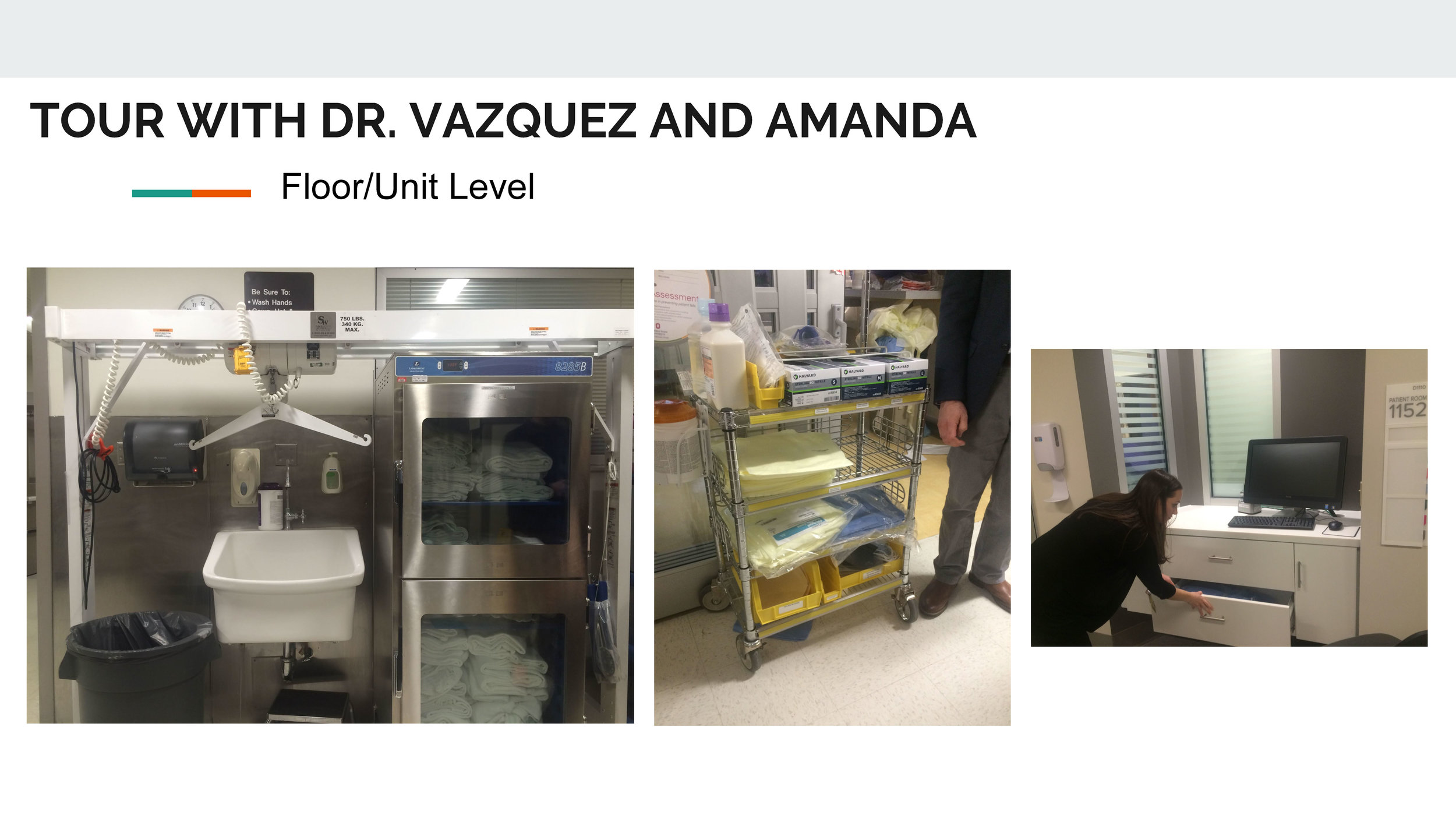
As a class of graduate students from the department of Design, Occupational Therapy, Health and Rehabilitation Sciences, Biomedical Informatics, and Industrial Systems Engineering with a focus on Human factors, we had to prepare ourselves with the working environment, and background studies surrounding ICU settings. The first phase of this studio's process was to immerse ourselves in secondary research and literature, and to attend expert lectures delivered by the core medical team. We were also given detailed tours of the existing surgical ICU units at the James, the Ross, and the University Hospital, OSU Campus.
UNDERSTANDING THE BASICS…
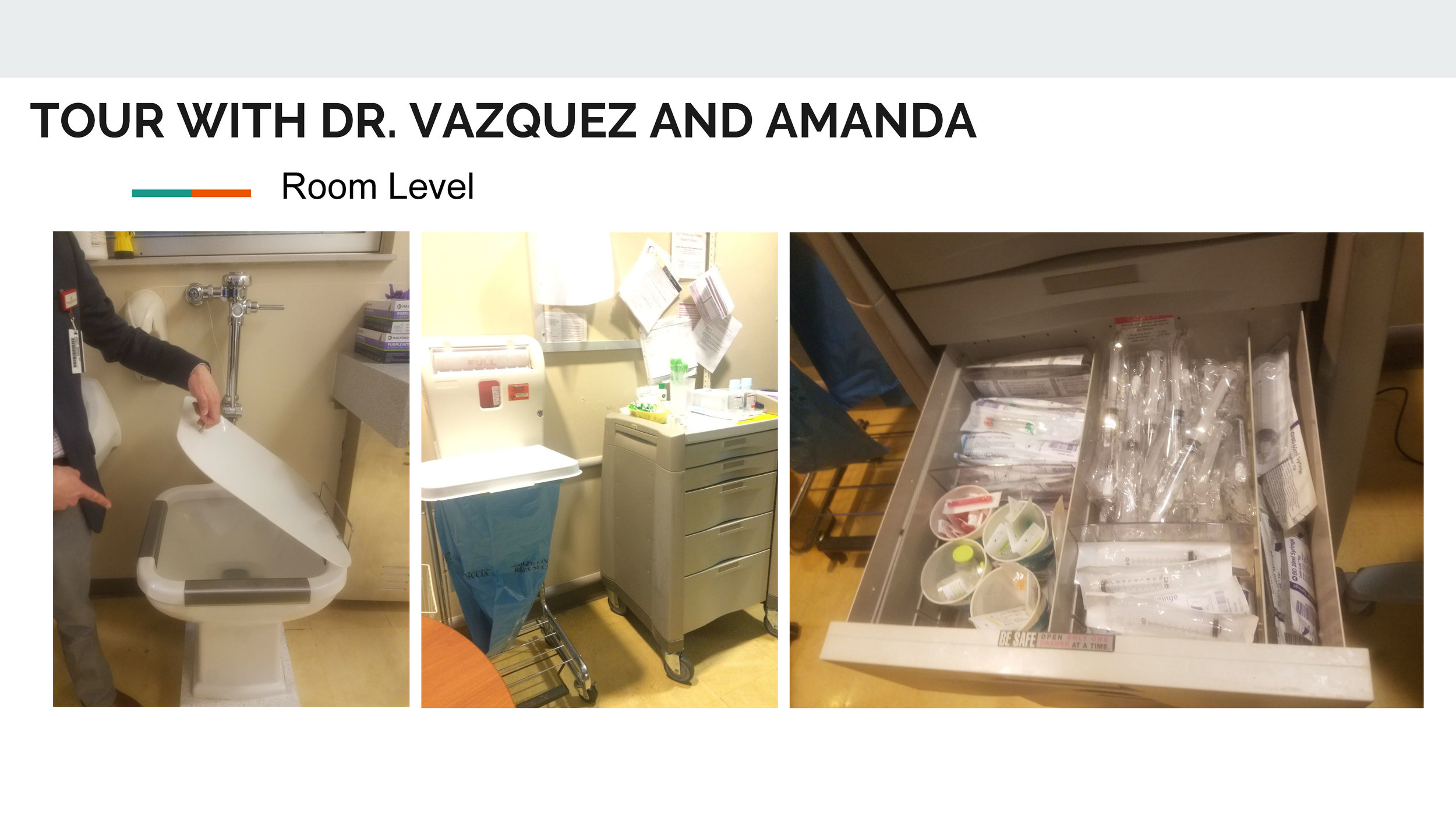
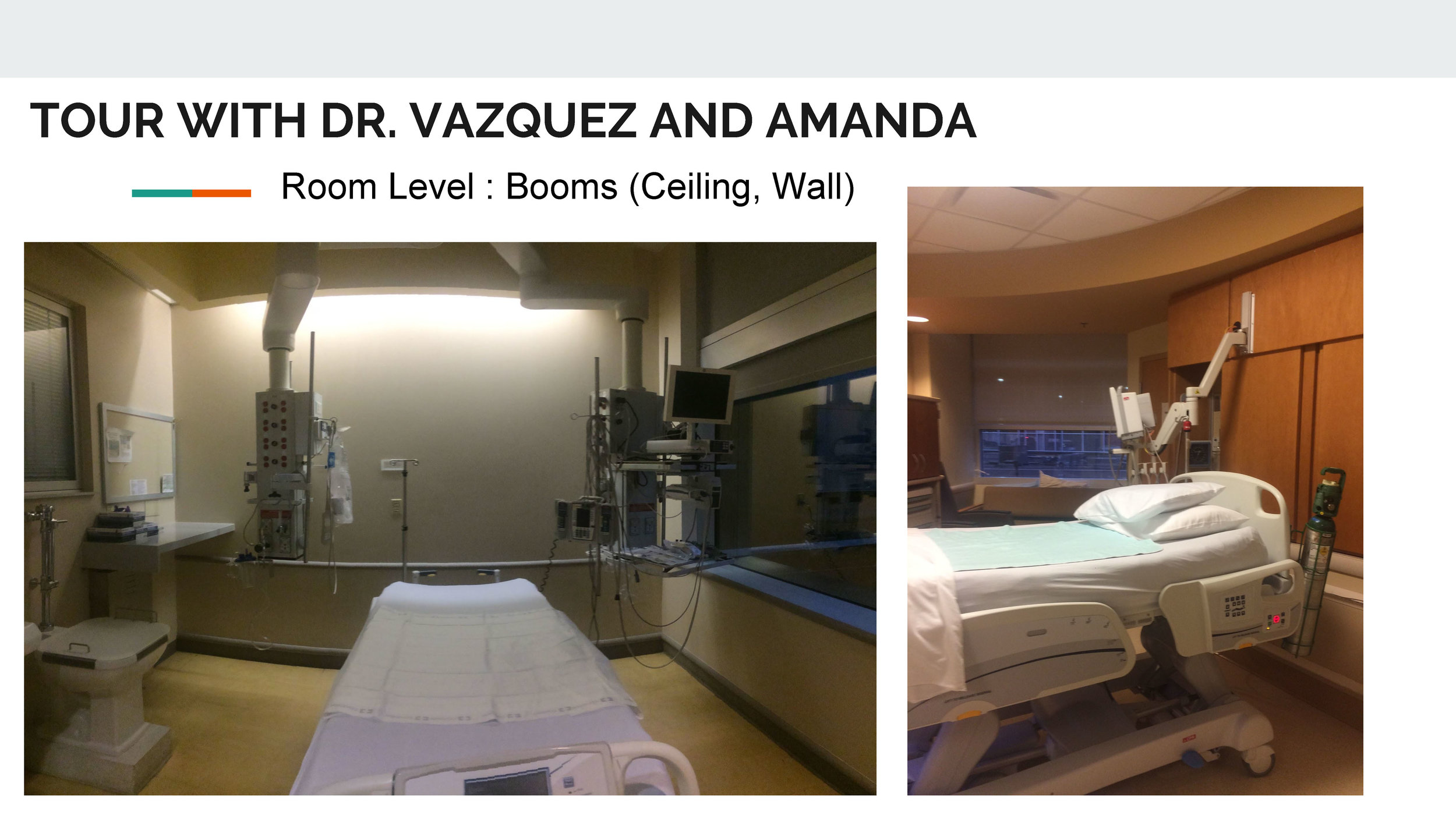
Dr. Vasquez and his team helped us with our initial understanding of medical processes, important information about procedures and the kind of infrastructure necessary to conduct them such as how the ICU unit works as such on the fronts of people experiences (where the nurses stations are and how they can watch over the patients, where the family is allowed, etc.), medical legalities (privacy of patients, HIPAA rules, etc.), and other building codes required on premises. This in-depth tour combined with lectures and secondary literature that was provided to us helped us get the basics of the working of a hospital in a holistic way before moving into Phase-2 where the workshops and co-design processes happen.
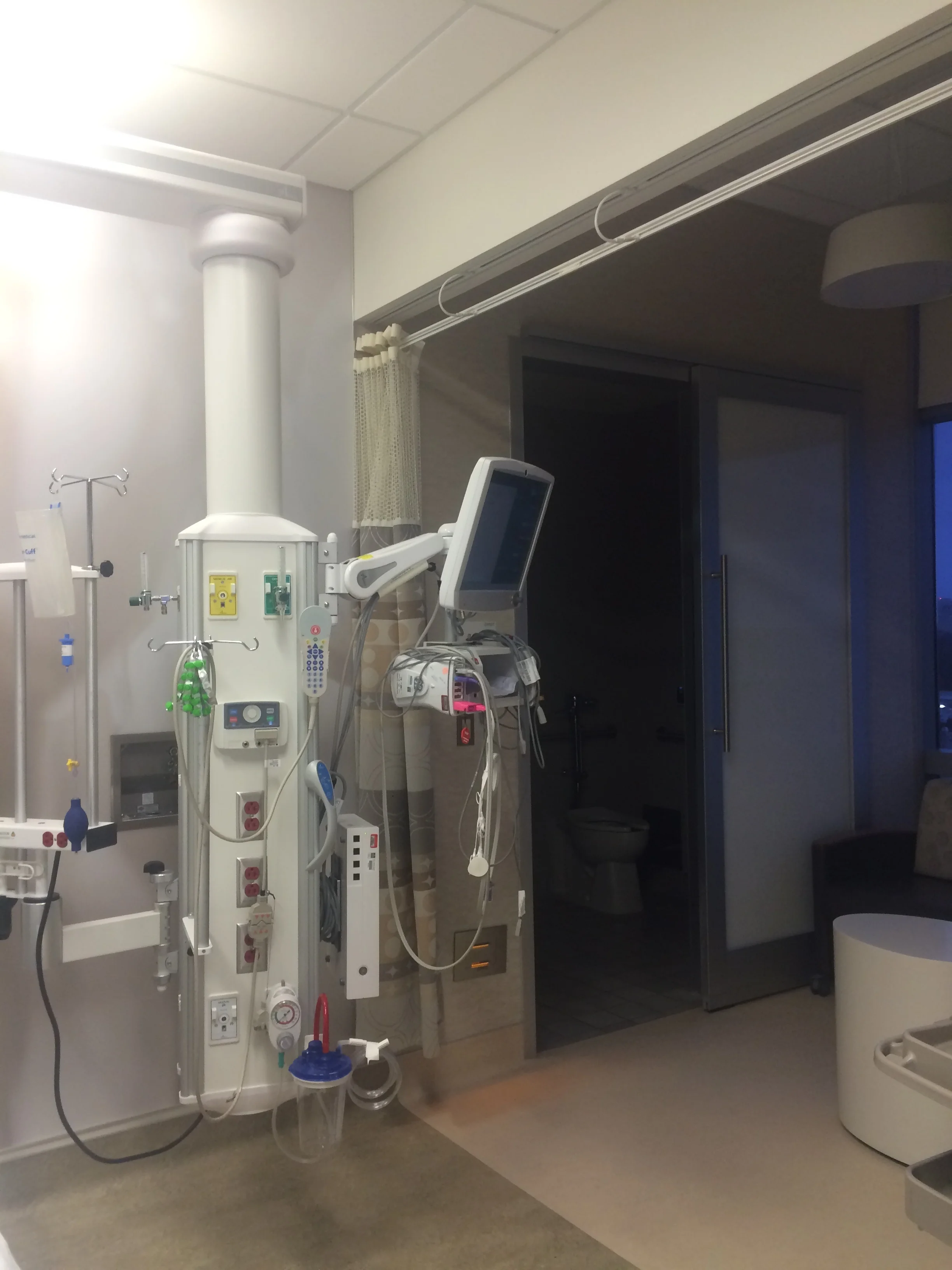
(above) Images from the tour of current ICU facilities between three different buildings of OSCMC— they had different degrees of upgrades, space layouts, and infrastructure additions based on when they were built. Each of these situations come with a specific set of issues and advantages. It’s imperative to understand these spaces completely before going to the next step in the process.
PHASE-2 | WORKSHOPS
Phase-2 consists of three different co-design workshops:
Workshop 1: Understanding the current experience
Workshop 2: Prioritization of opportunities
Workshop 3: Exploring future scenarios of use
Phase-2 | Workshop 1 : Understanding the Current Experience
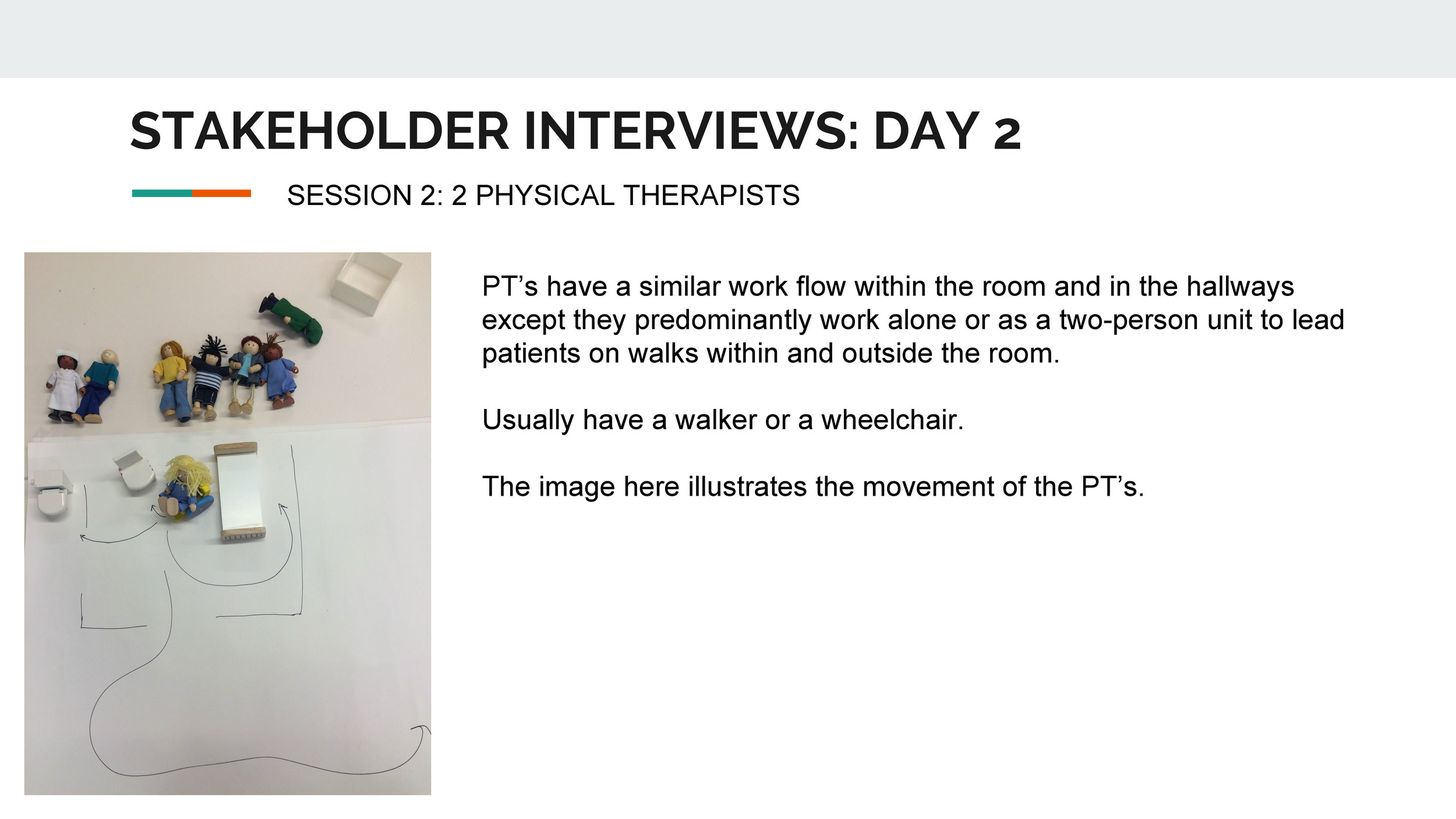
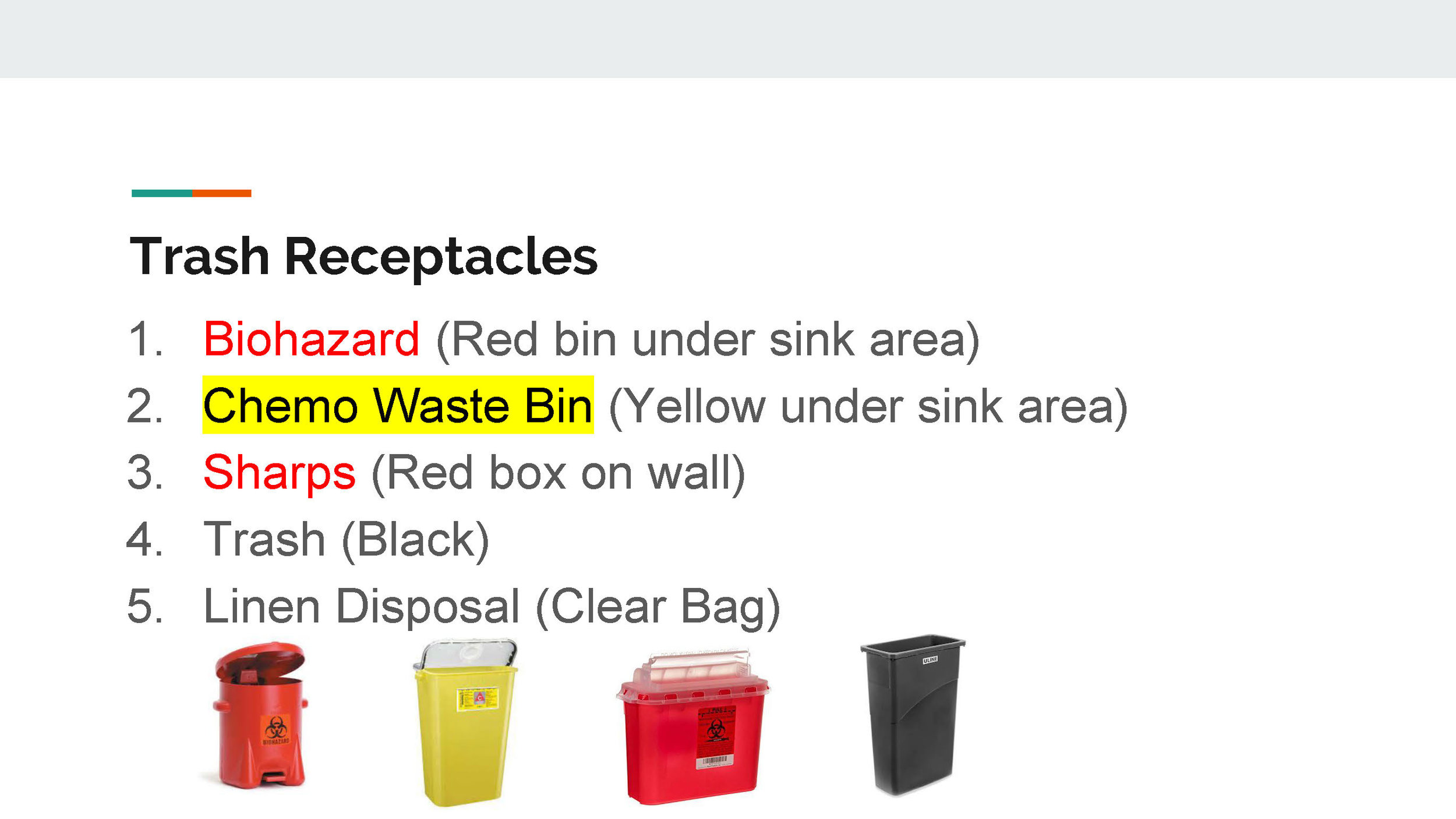
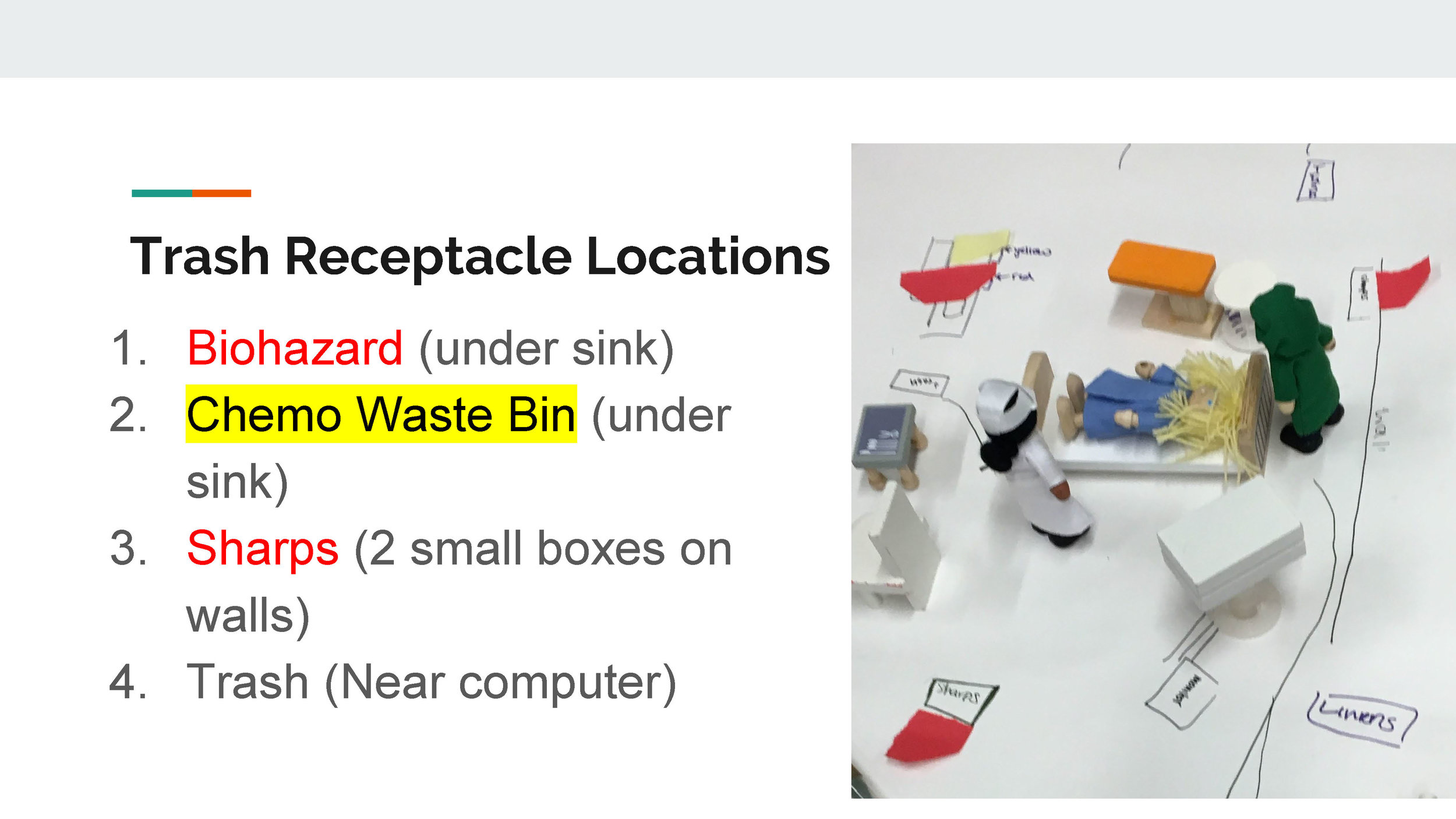
For the first workshop, four groups were established to understand the experiences of four main stakeholder groups: Patient, Family, Staff, and Trash Disposal and Hygiene. In this round of workshops, I was a part of 'Team Trash' along with Mike, Steven, and James. Our team aimed to elicit people's experiences surrounding waste generation and disposal at the ICU ward, the working points and current concerns of the systems and products in use surrounding this. We interviewed many staff members like Nurse Practitoners (NP), MDs, Patient Care Assistants (PCA), Respiratory Therapists (RTs) etc.
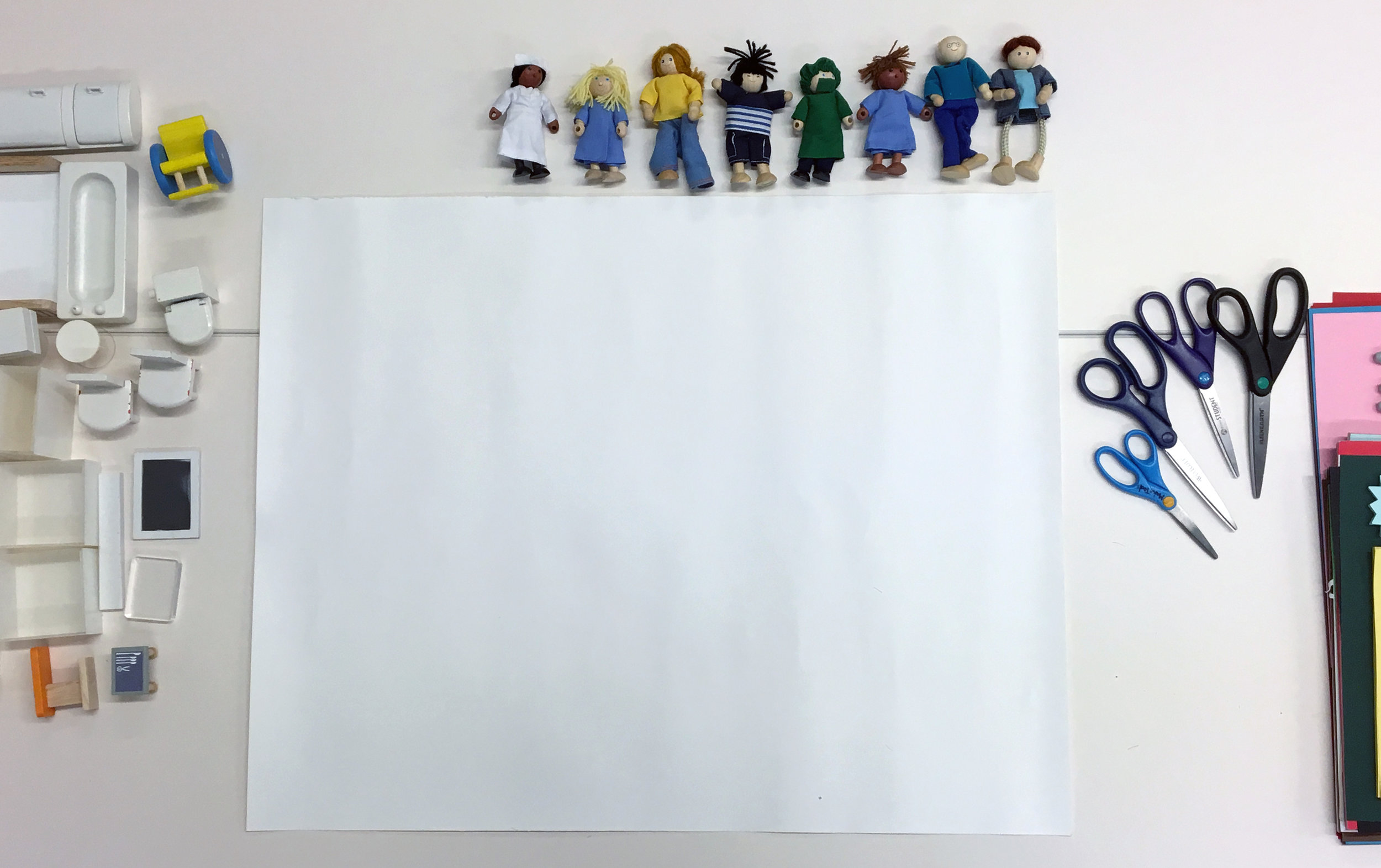
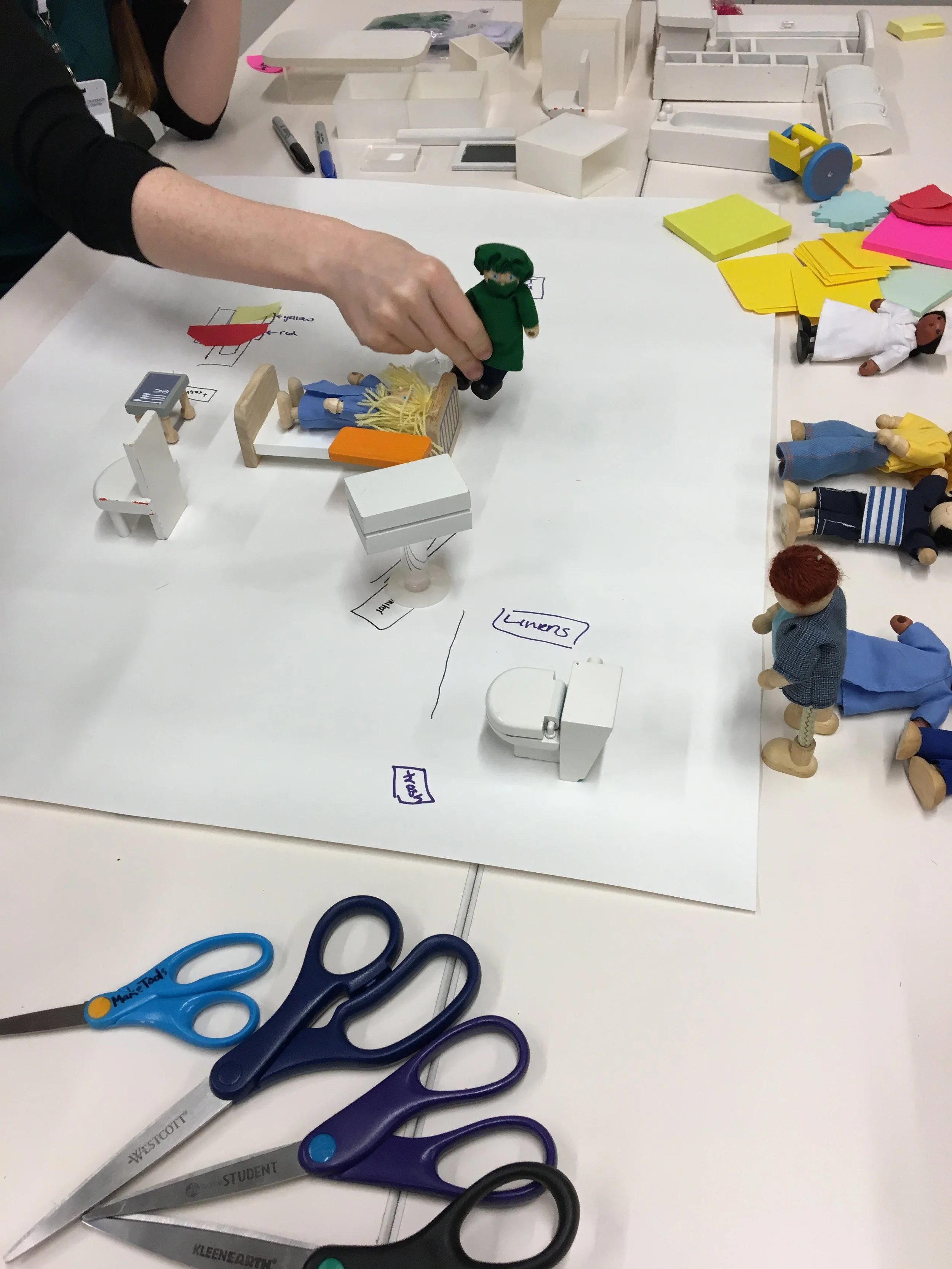
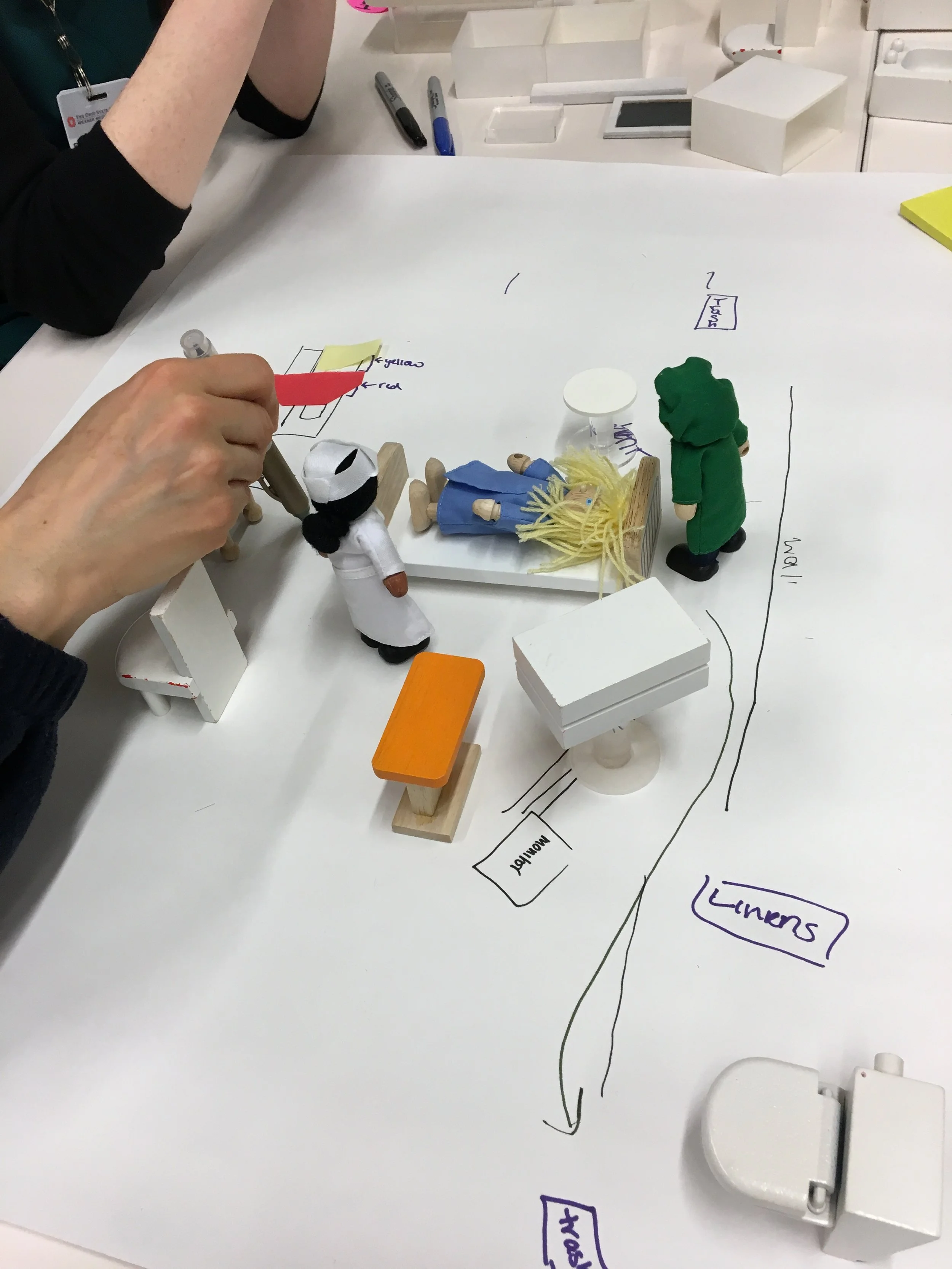
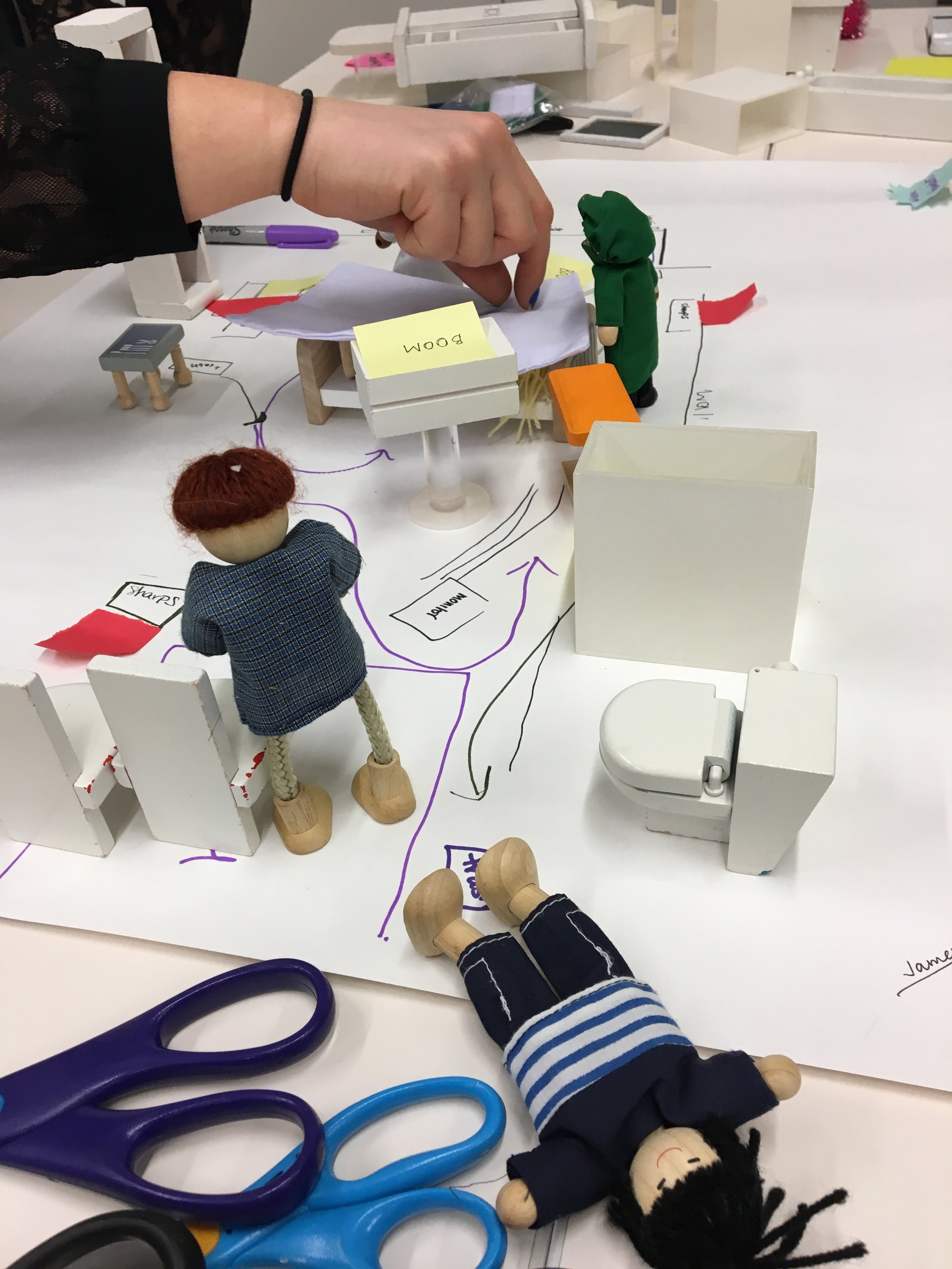
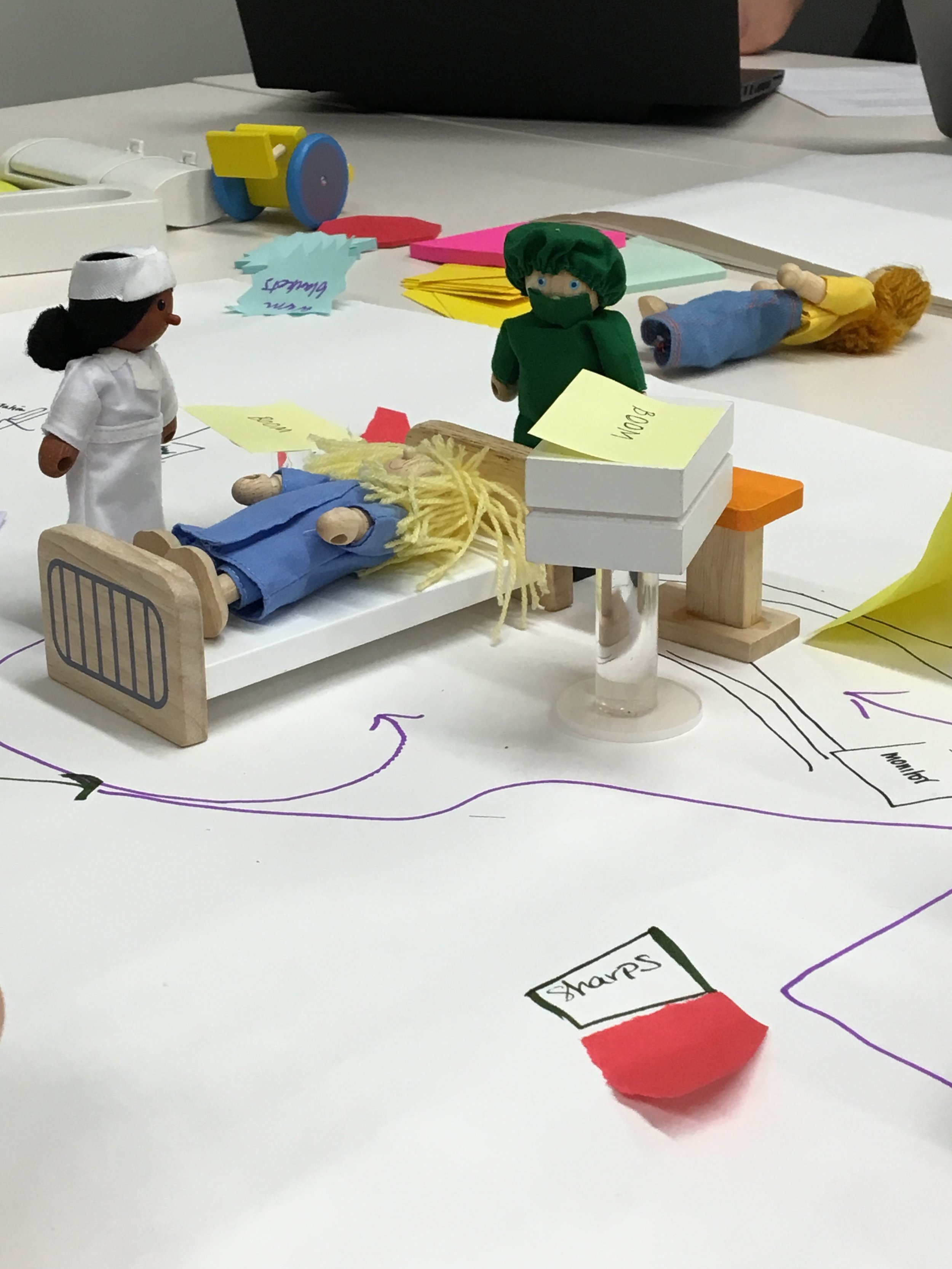
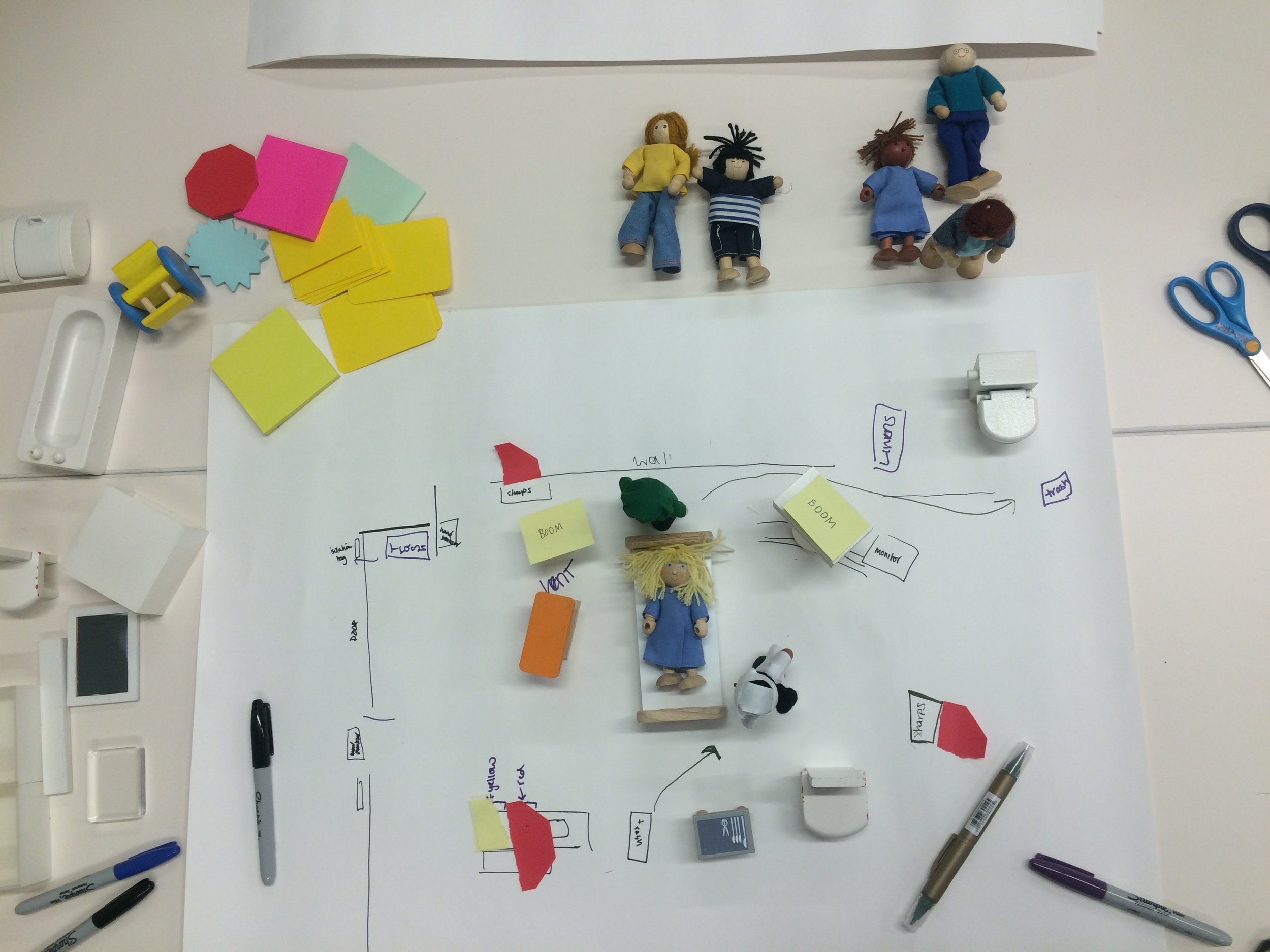
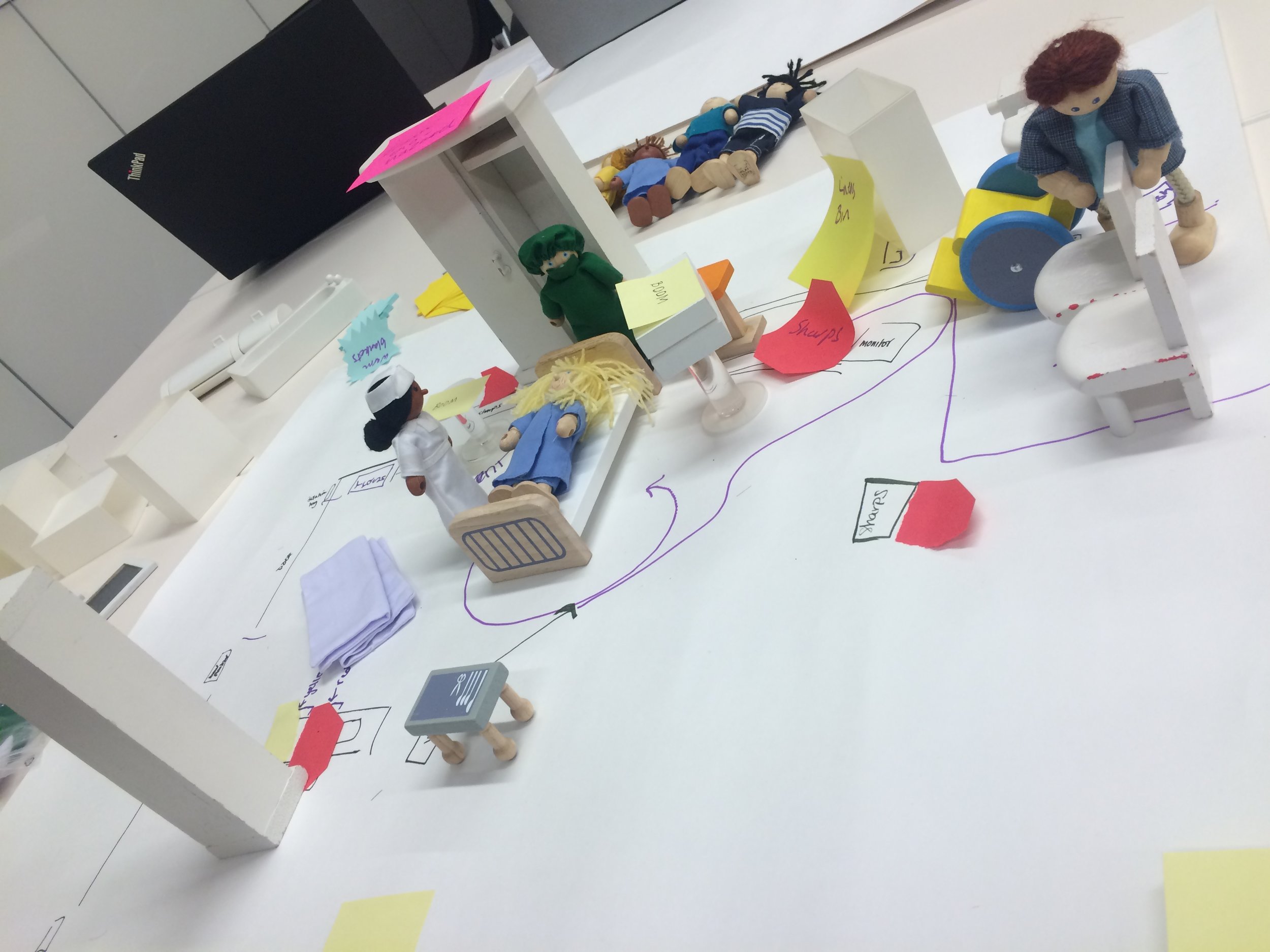
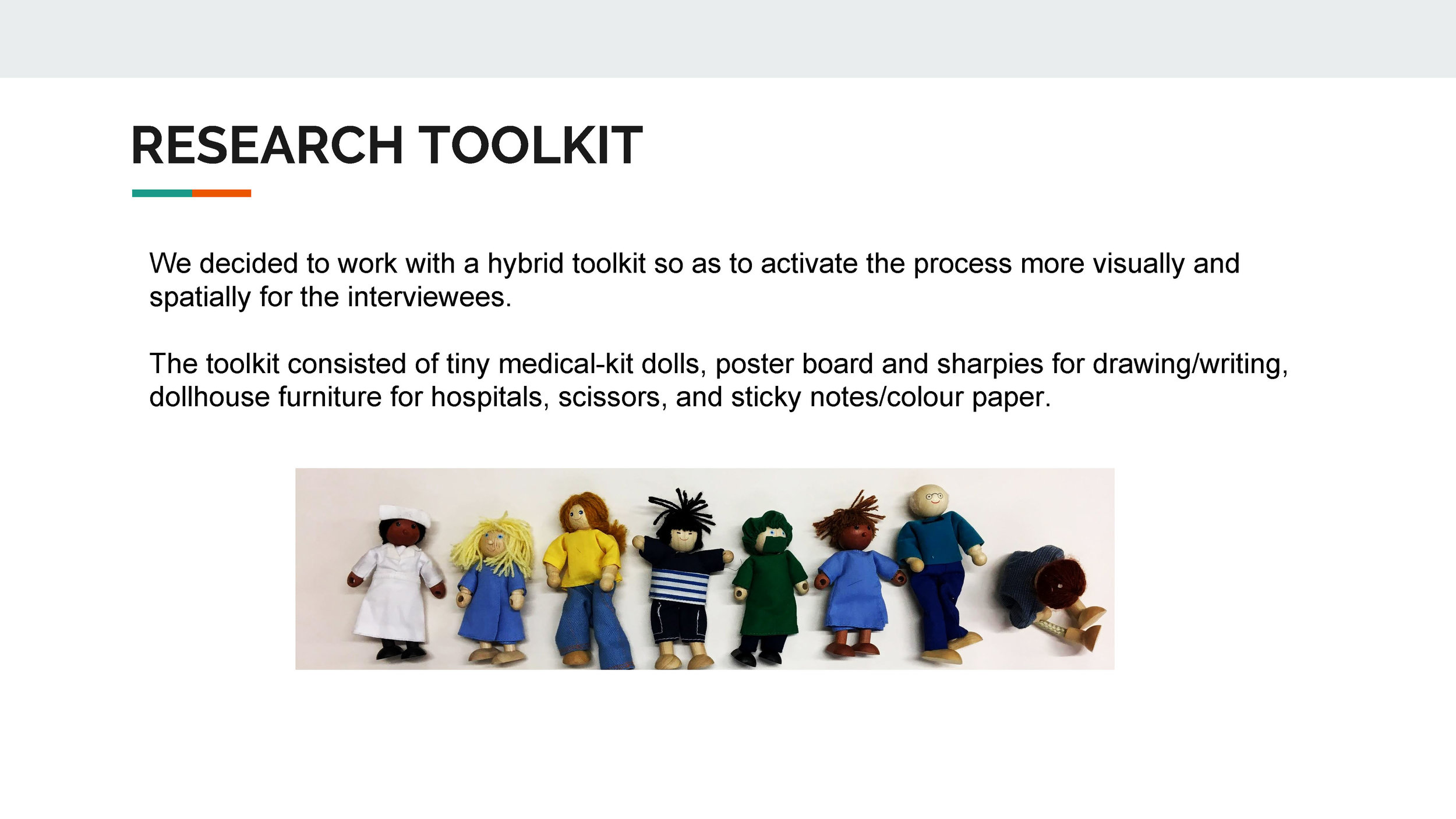
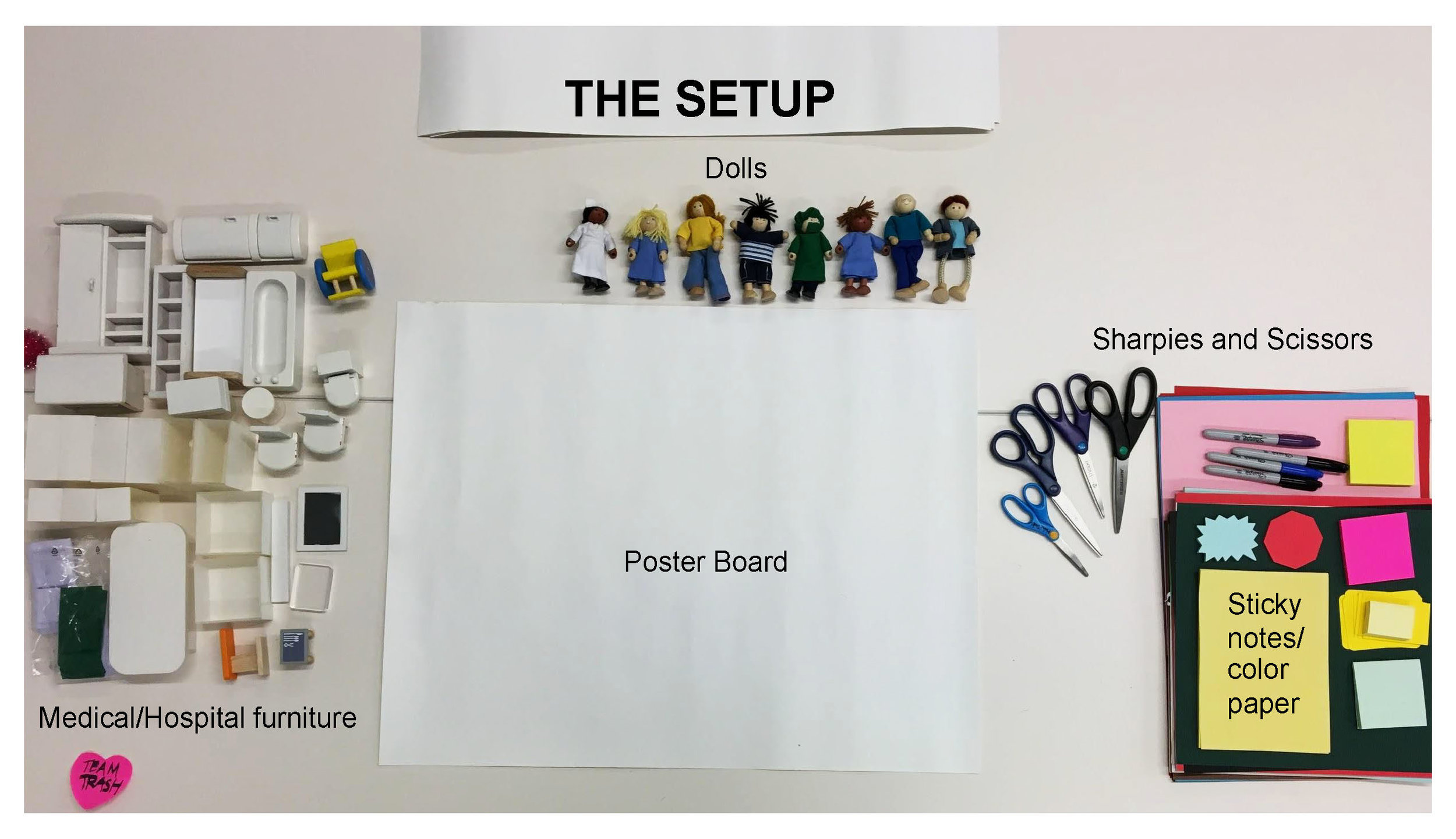
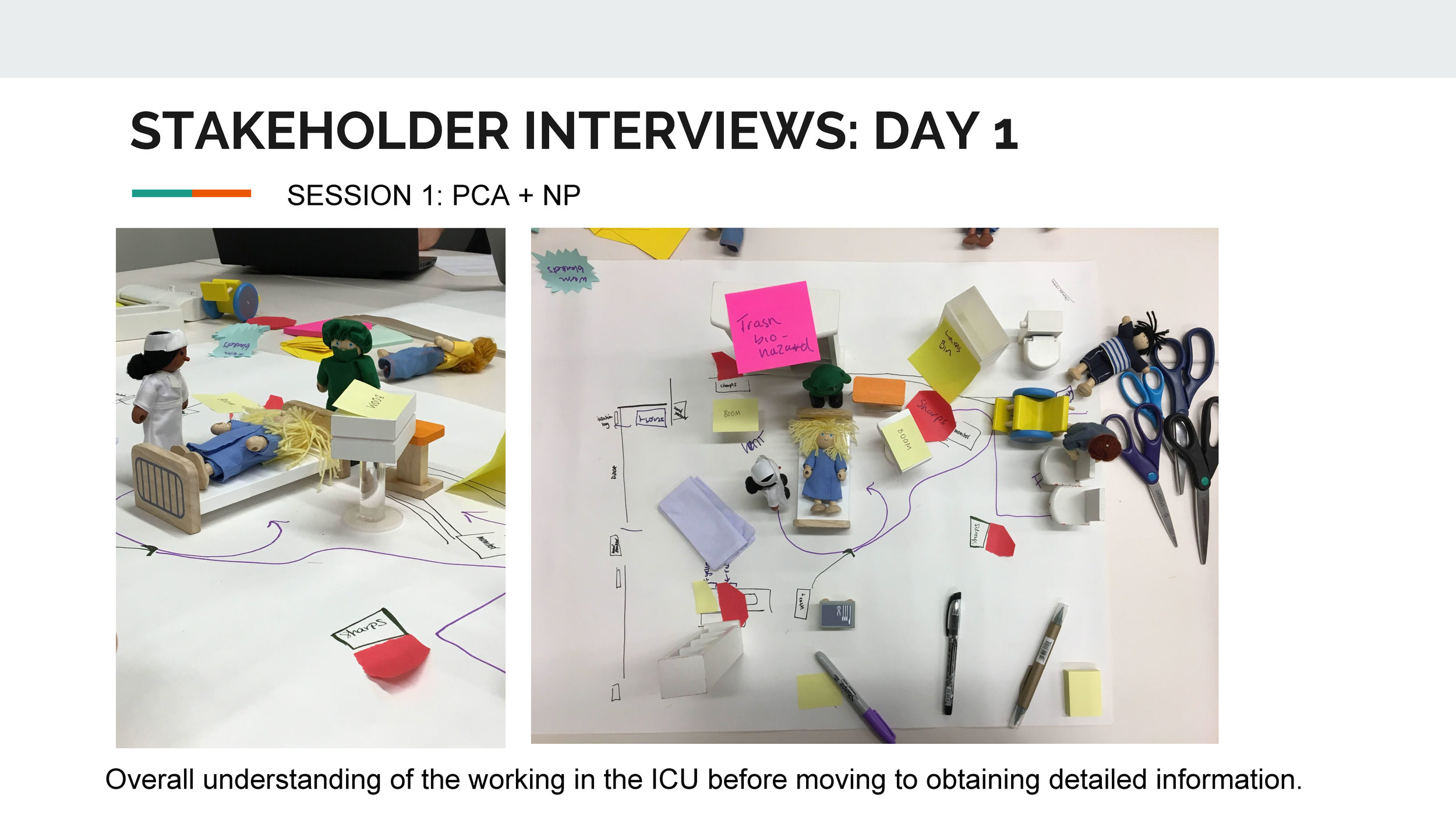
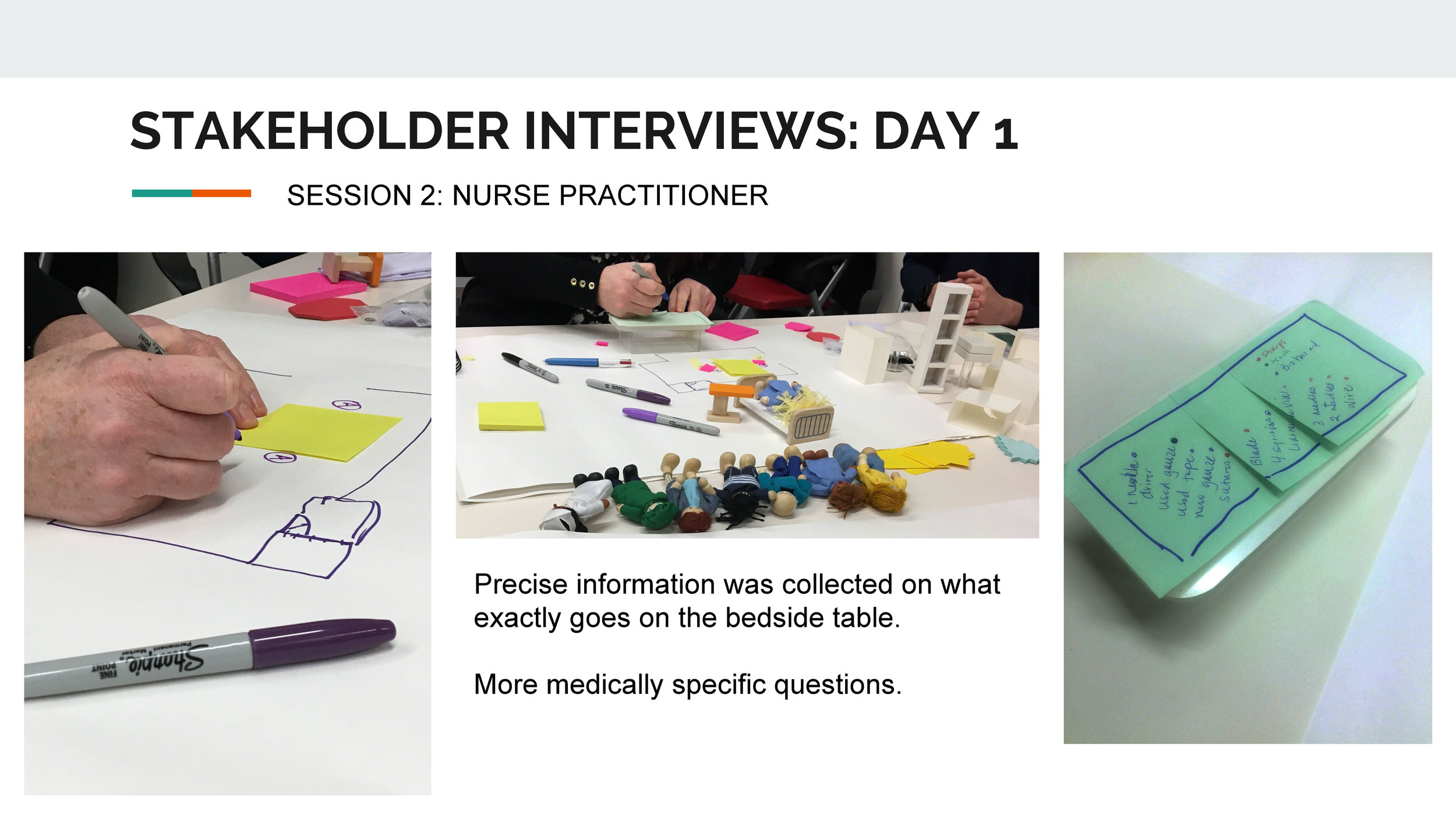
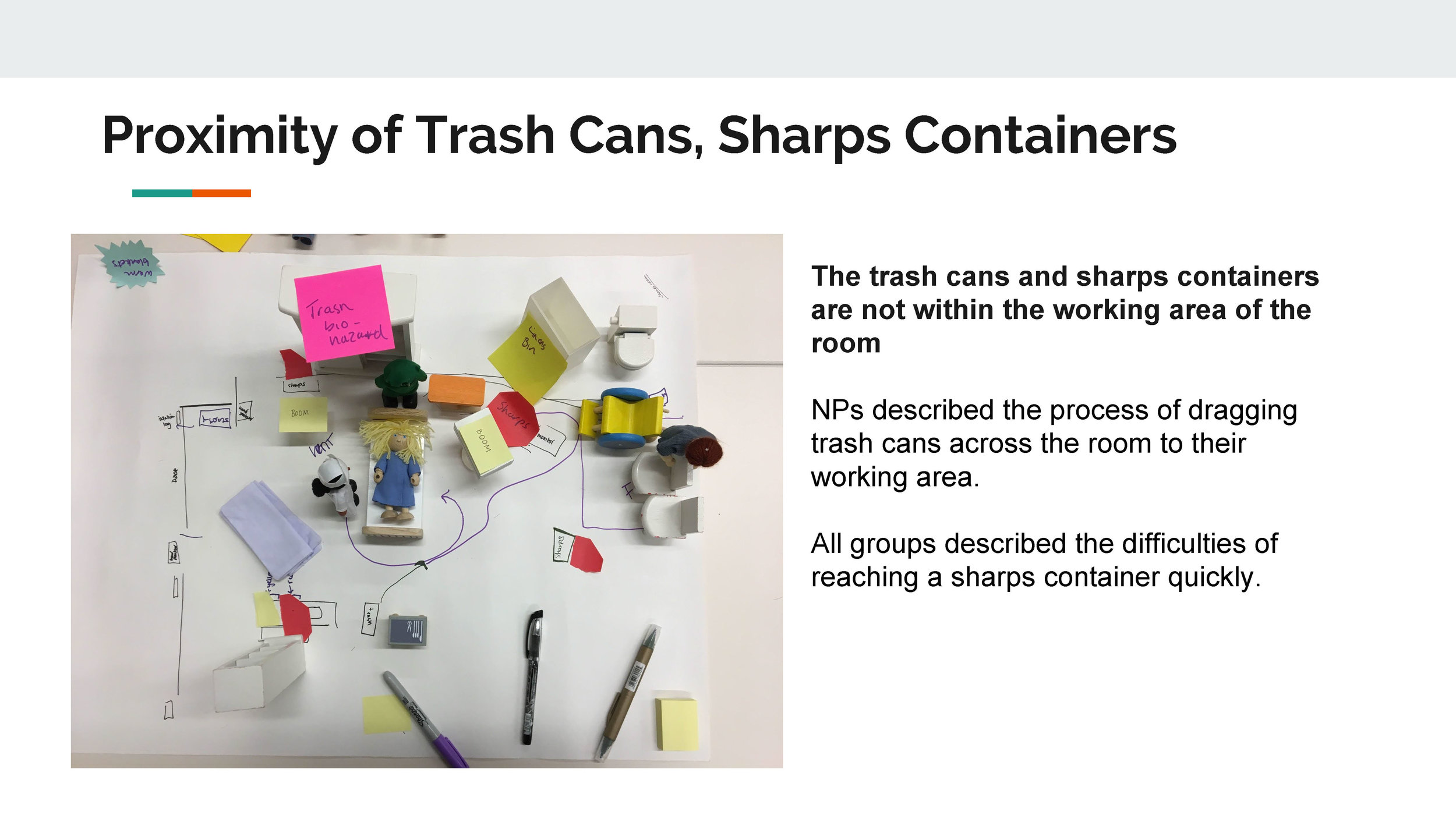
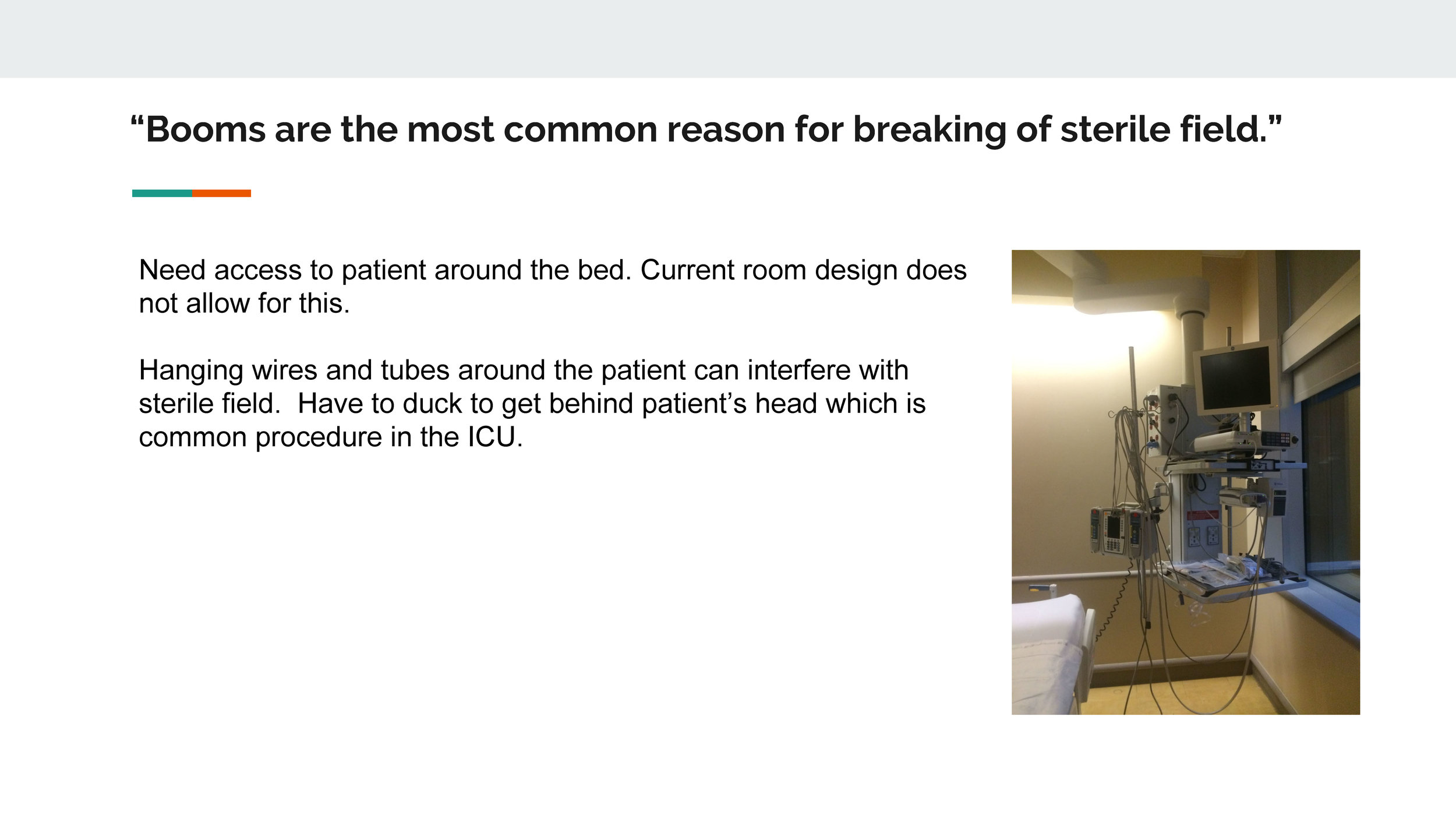
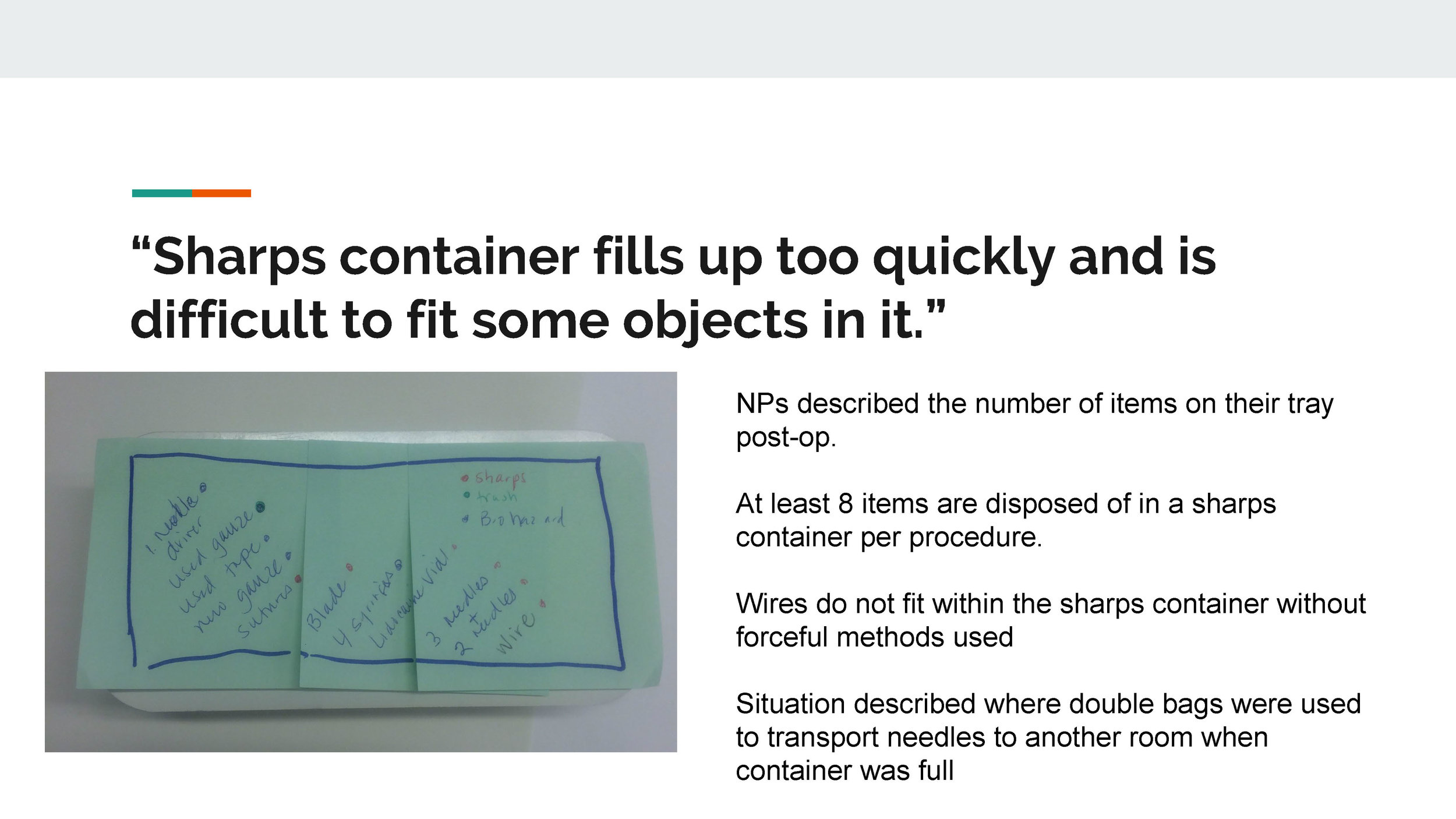
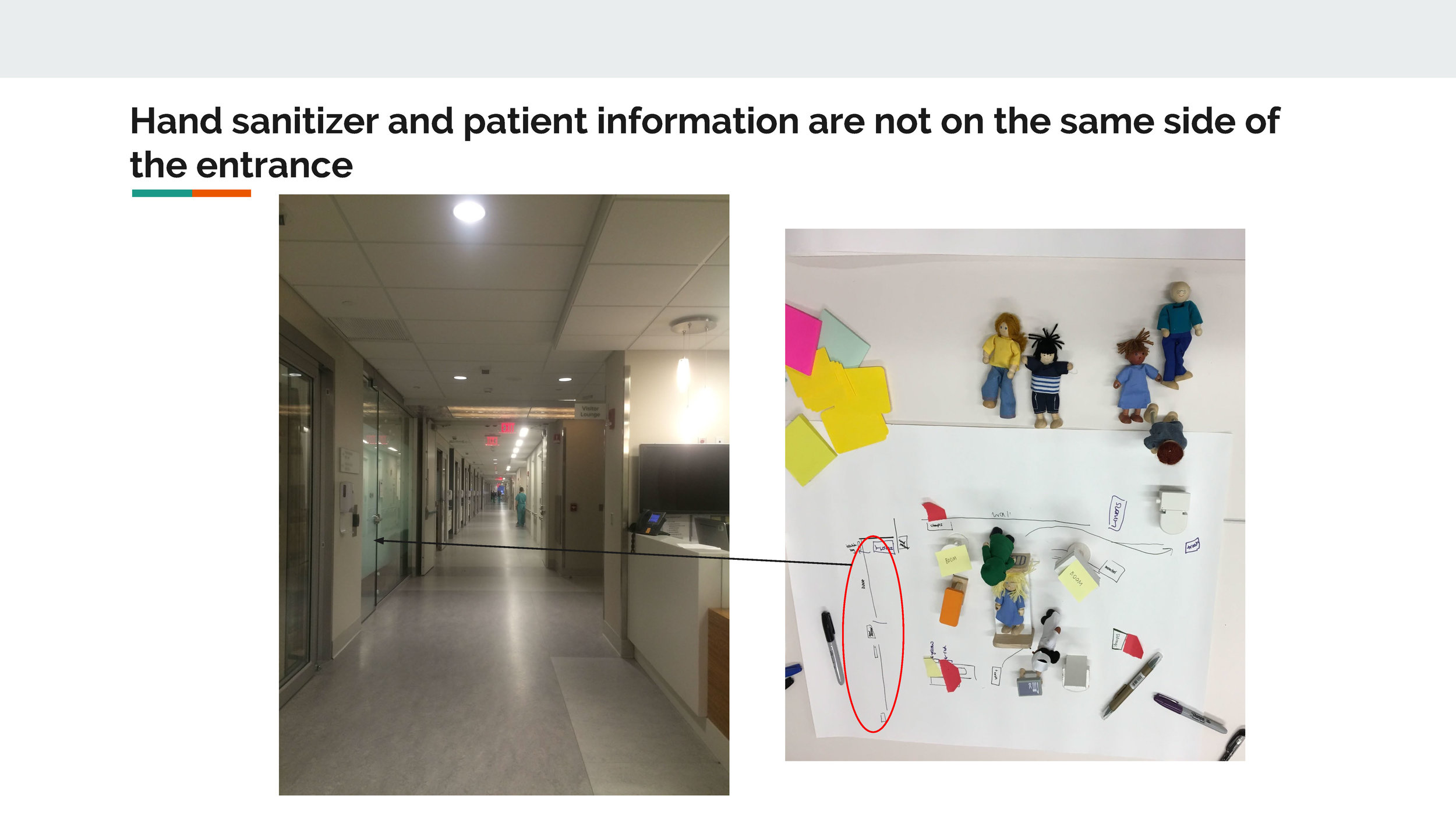
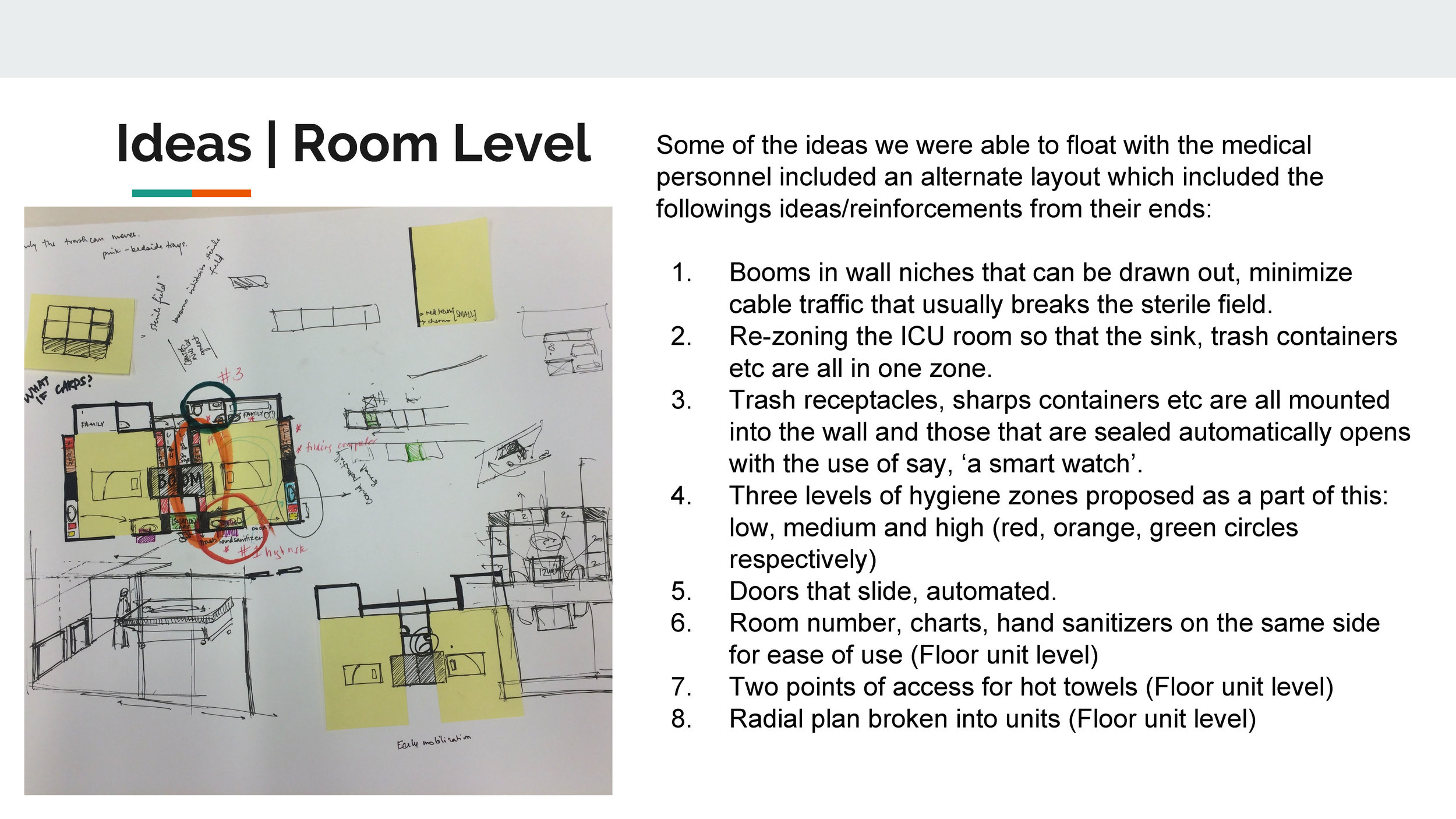
We provided the participants with a poster board, sharpies, post-its, dolls and doll house furniture to recreate their ICU working setting. This enabled them to recreate and explain their problems particular to waste generation and disposal. Each staff member or health care practitioner had their own personal experiences and preferences. We gained a lot of knowledge about the working patterns in the ICU and the existing infrastructure like booms, life support machines, pattern of movement in a surgery room, sterile field etc.
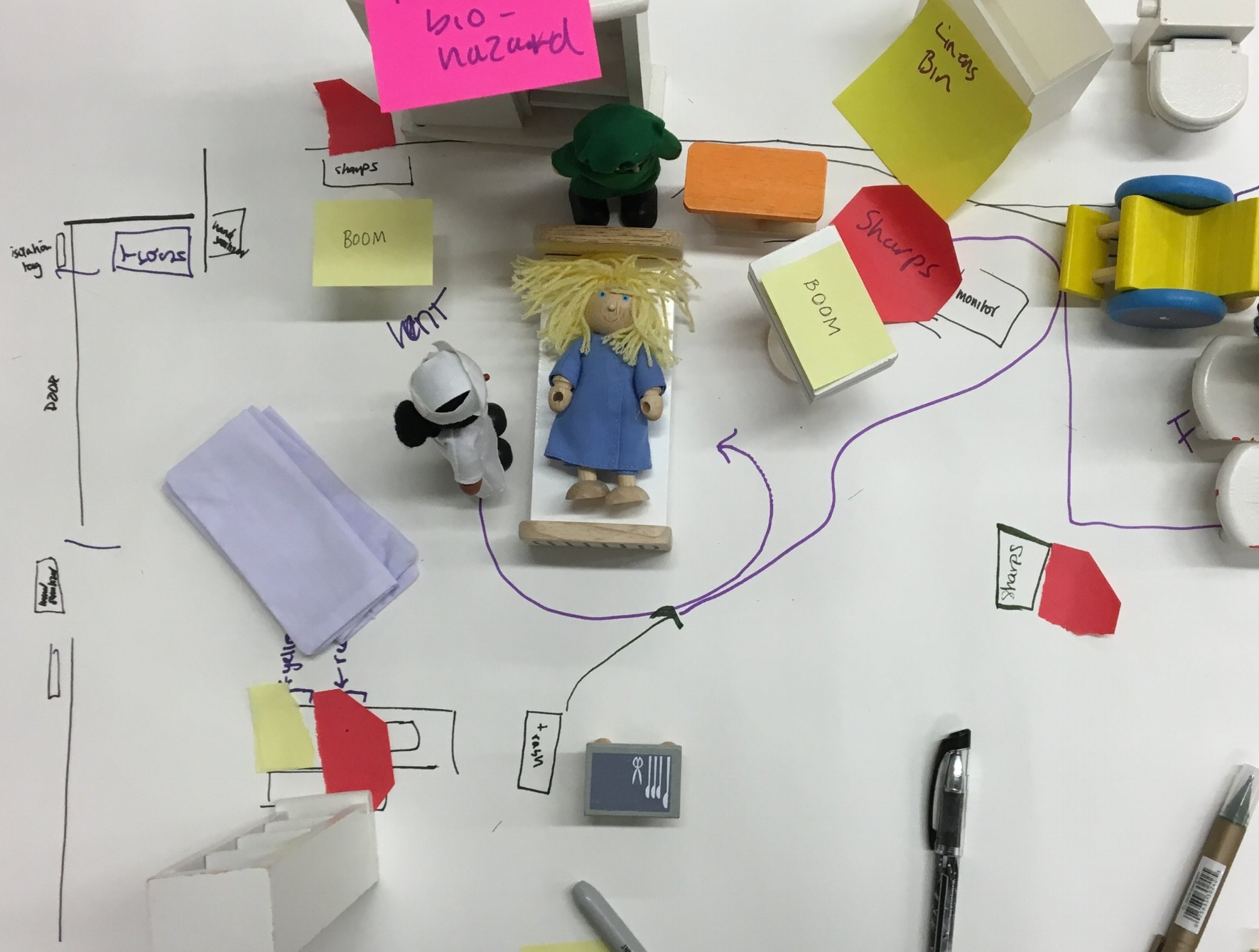

Between ourselves, we switched between the roles of being the note-taker, facilitator, and the person in-charge for photo-documentation. After facilitating a few interviews, I took on the role of visual note-taker. As a trained architect, I was able to cull main ideas from what the staff mentioned during the interviews and I proposed new, alternate plans to get their thoughts on it, particularly with respect to floor plans and risk zones.
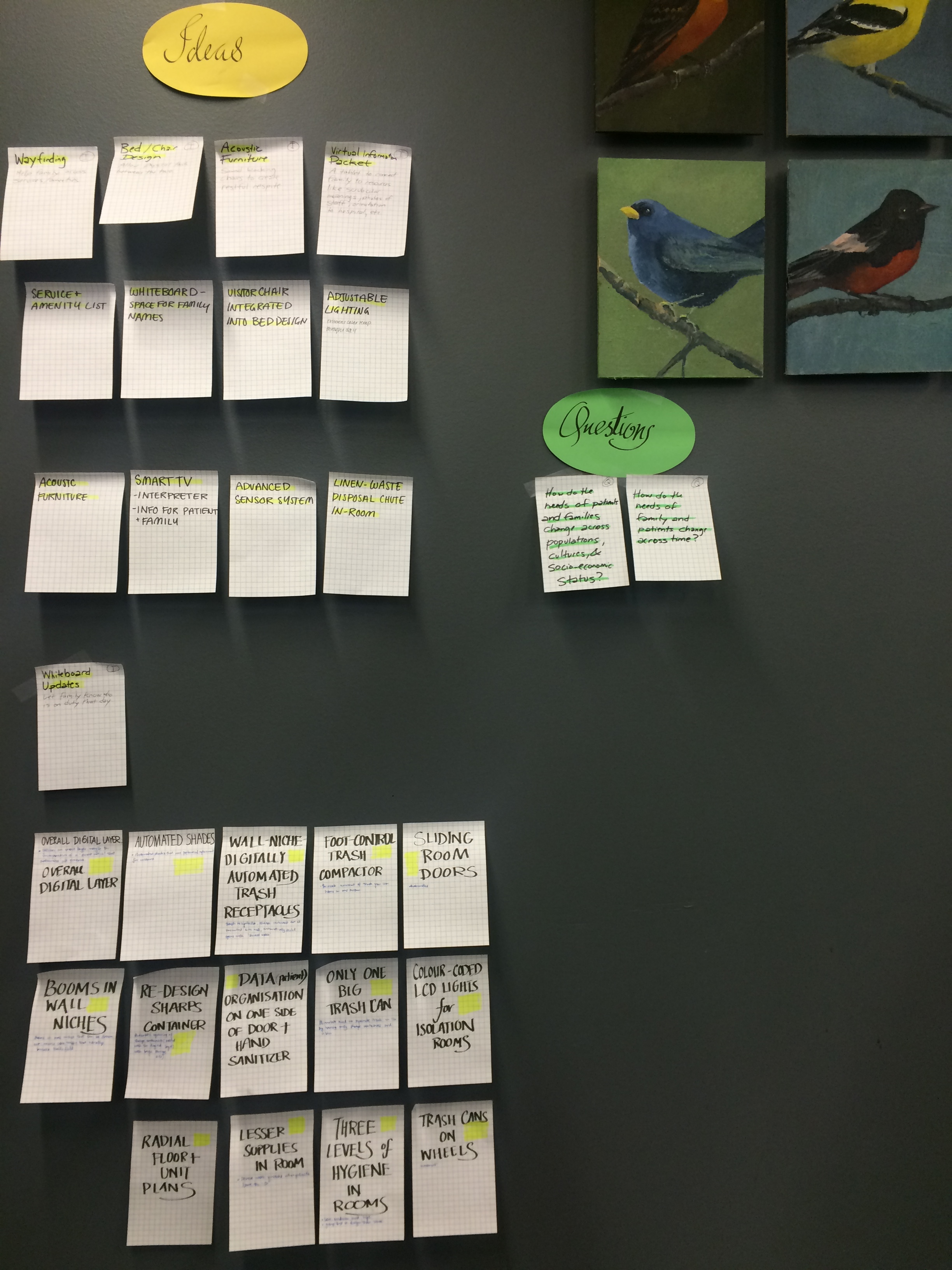
Each group presented our information about the current situation for each of the four main layer. Details of the trash and hygiene layer:

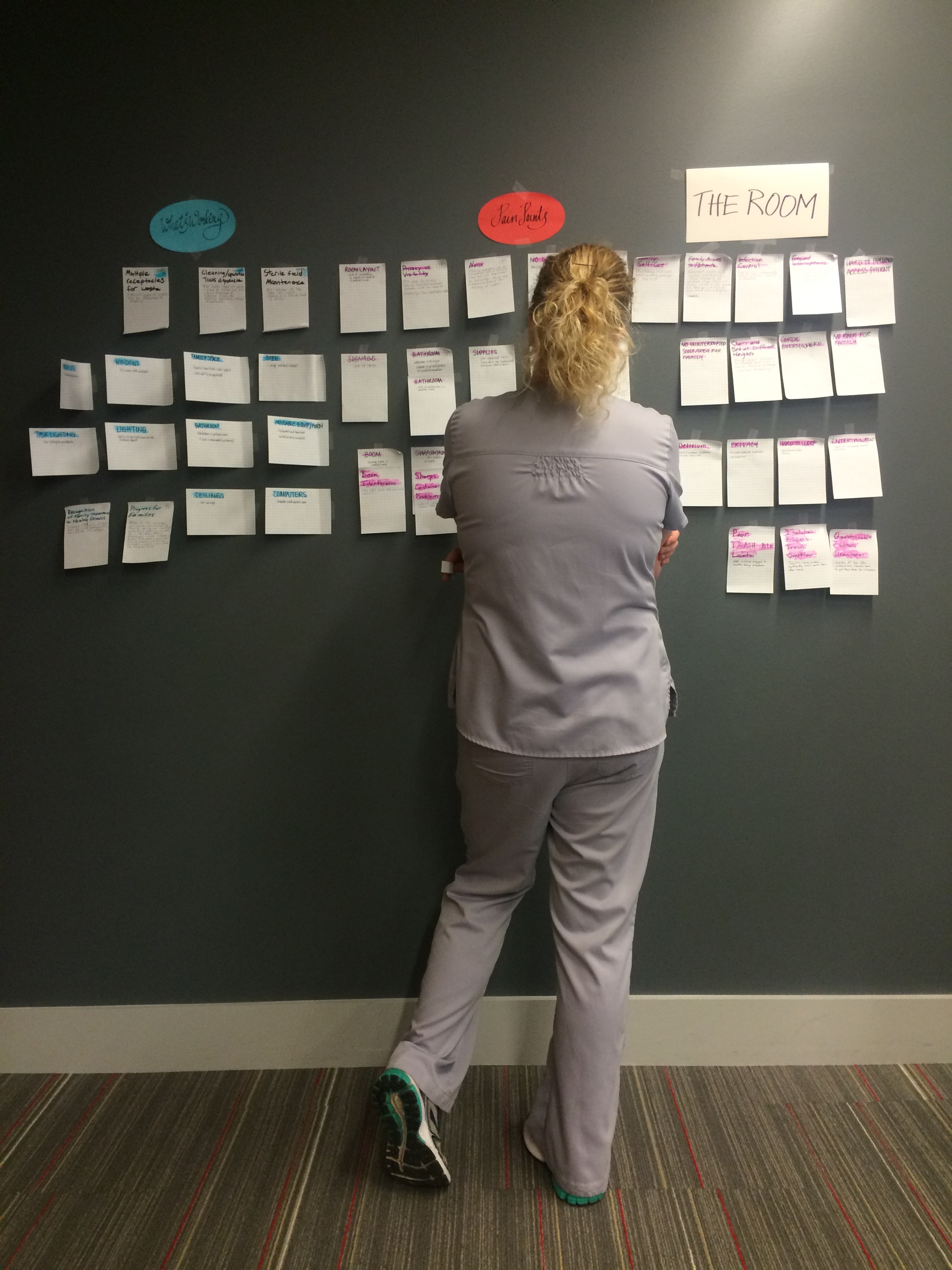
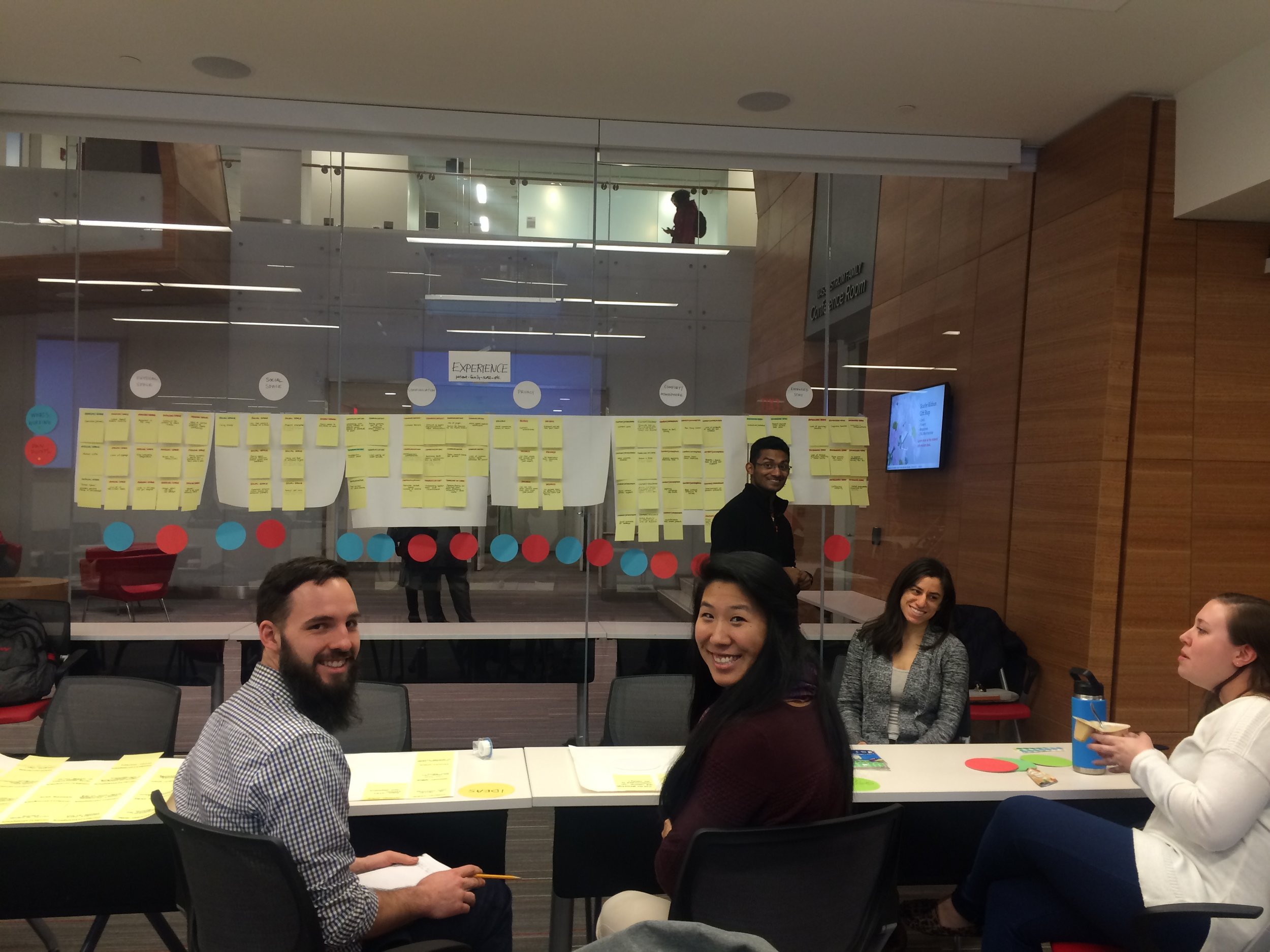
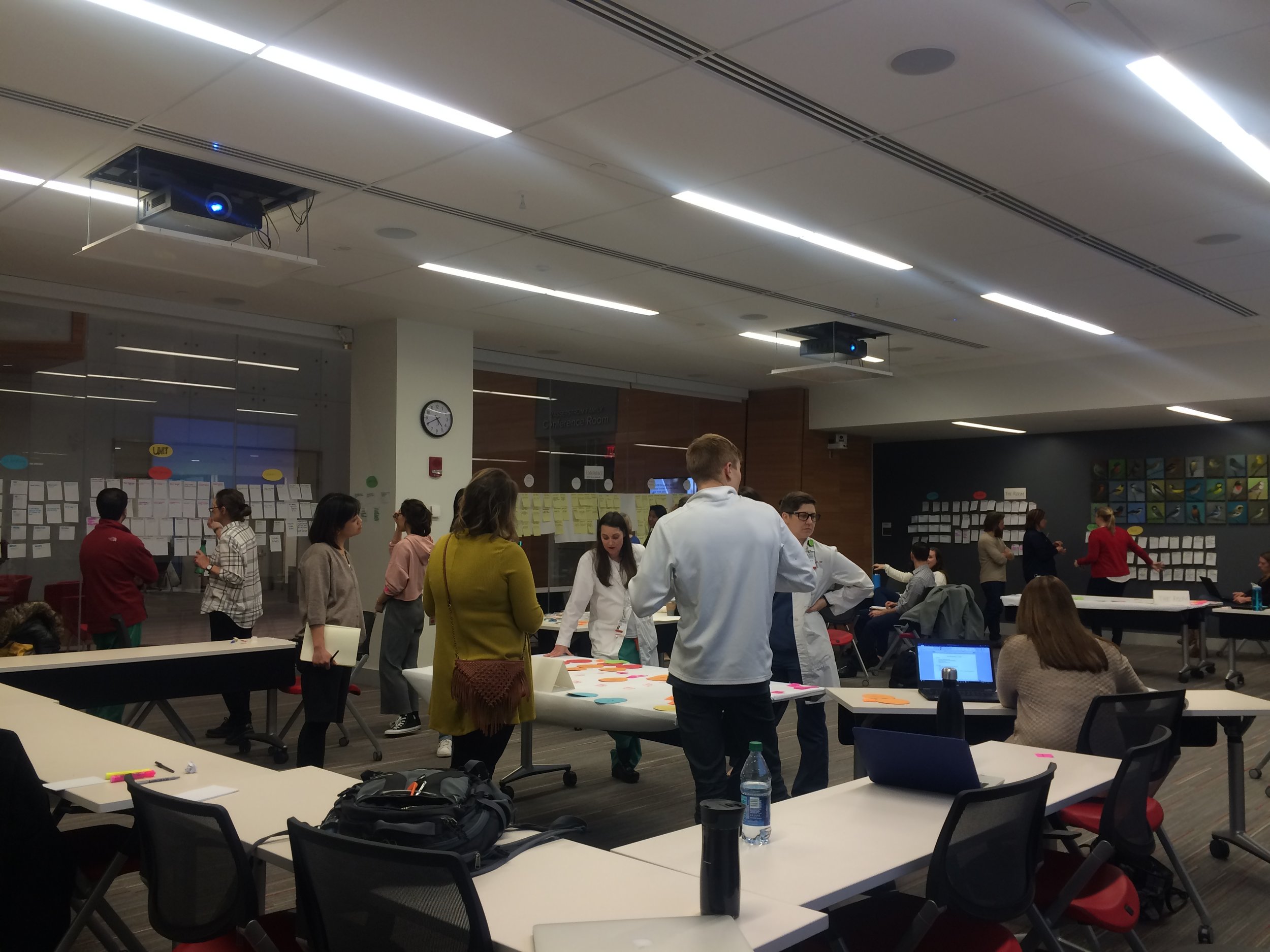
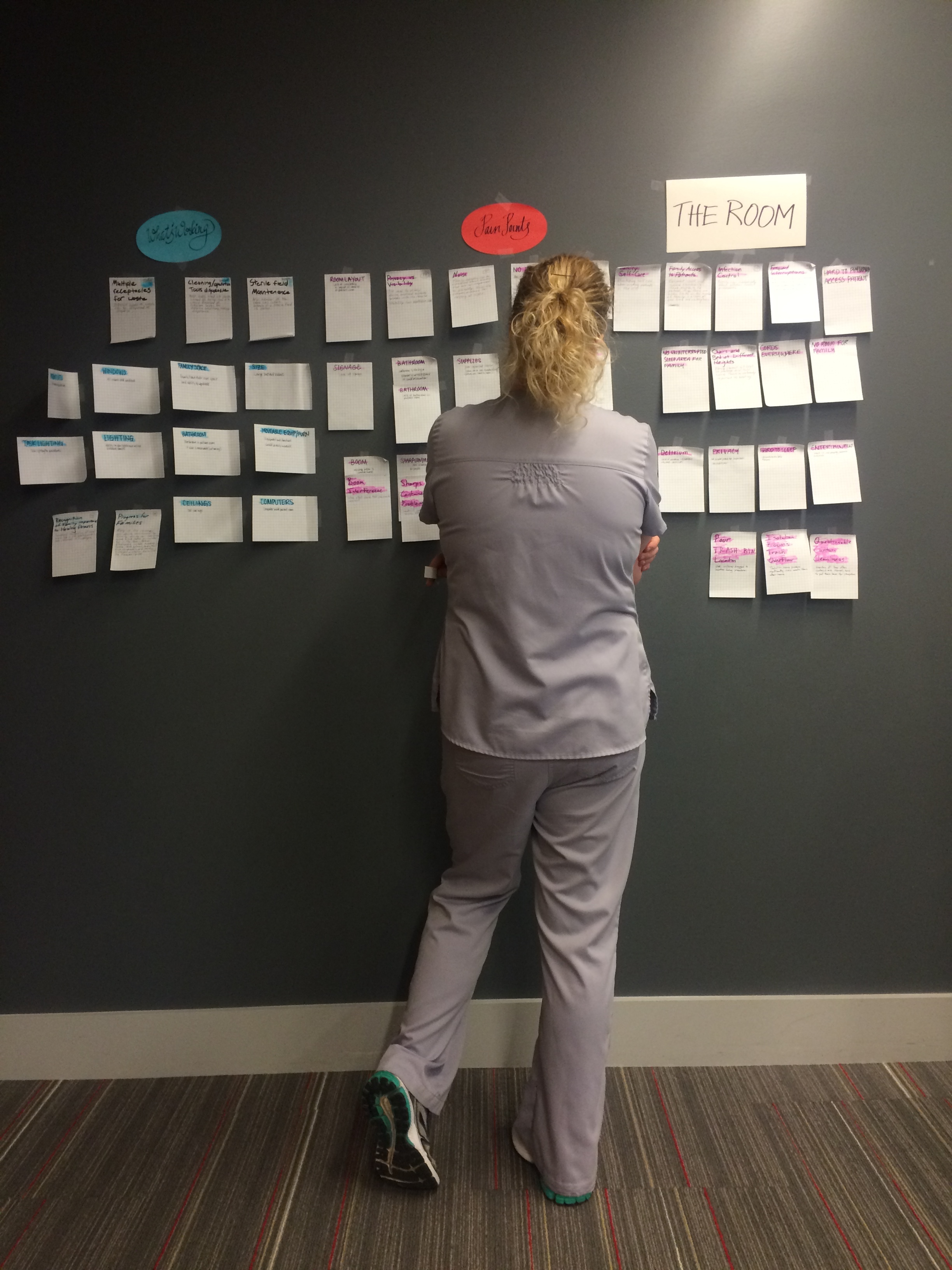
Phase 2 | Workshop-2 : Prioritization of Opportunities
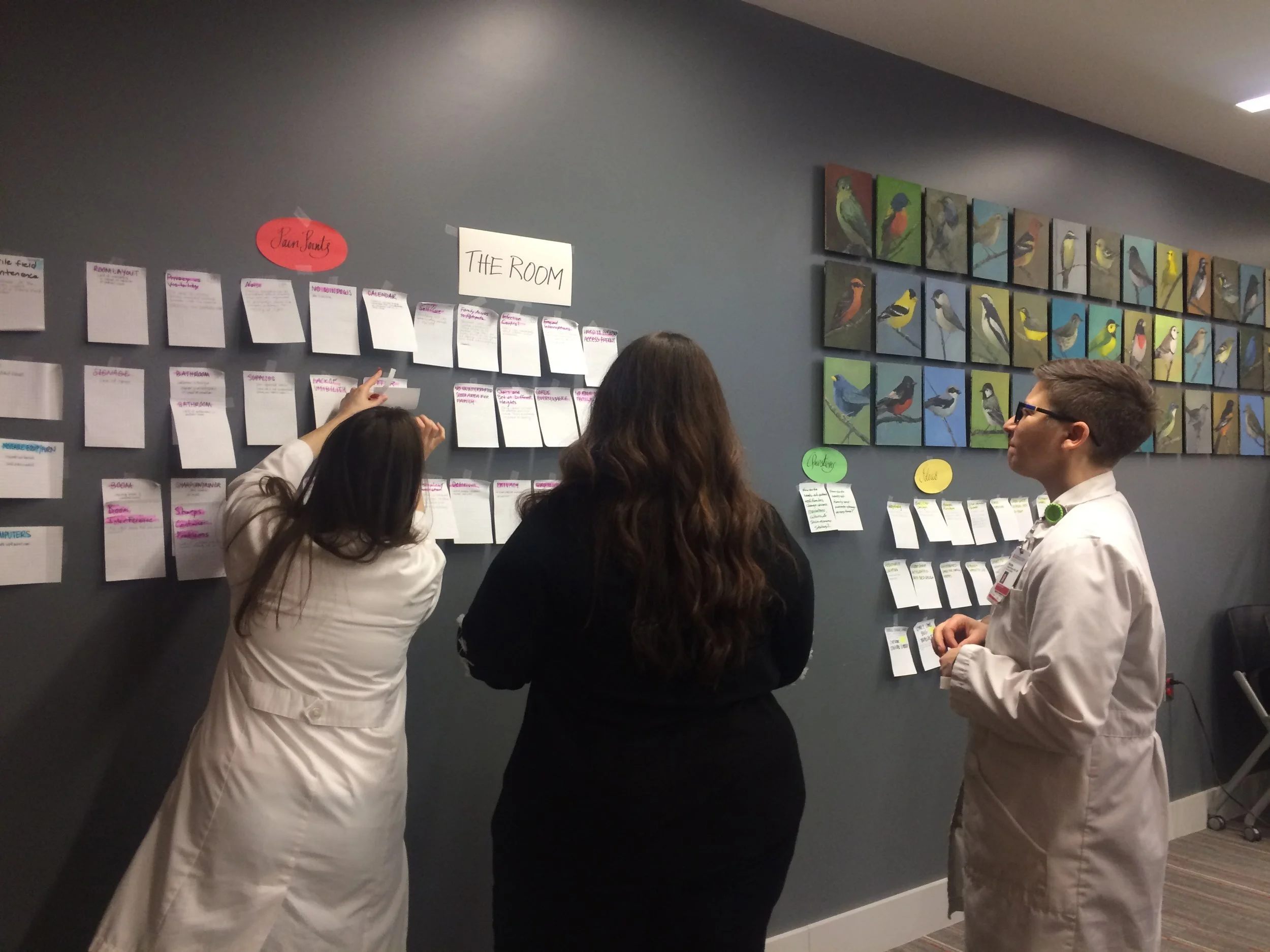
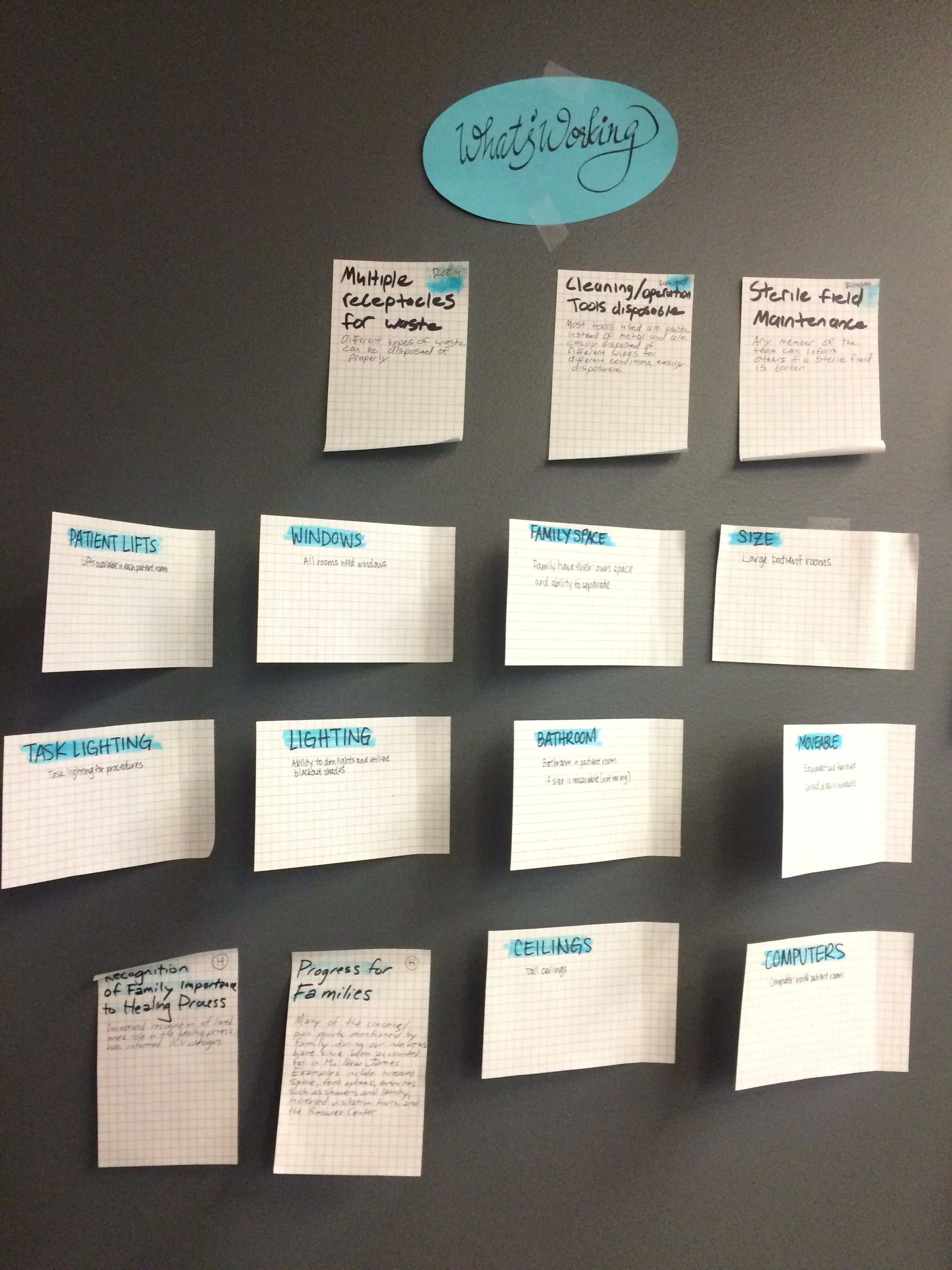
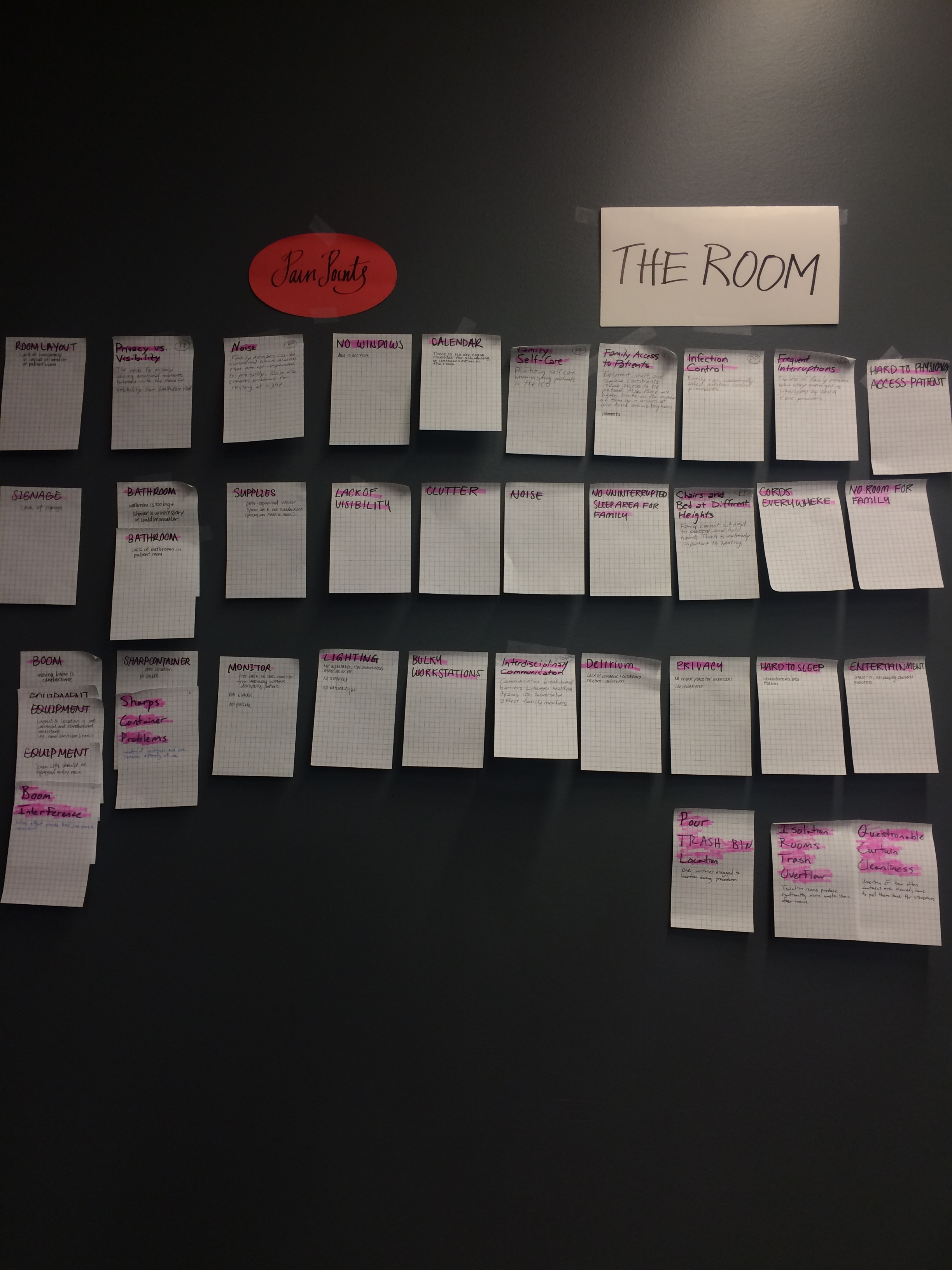
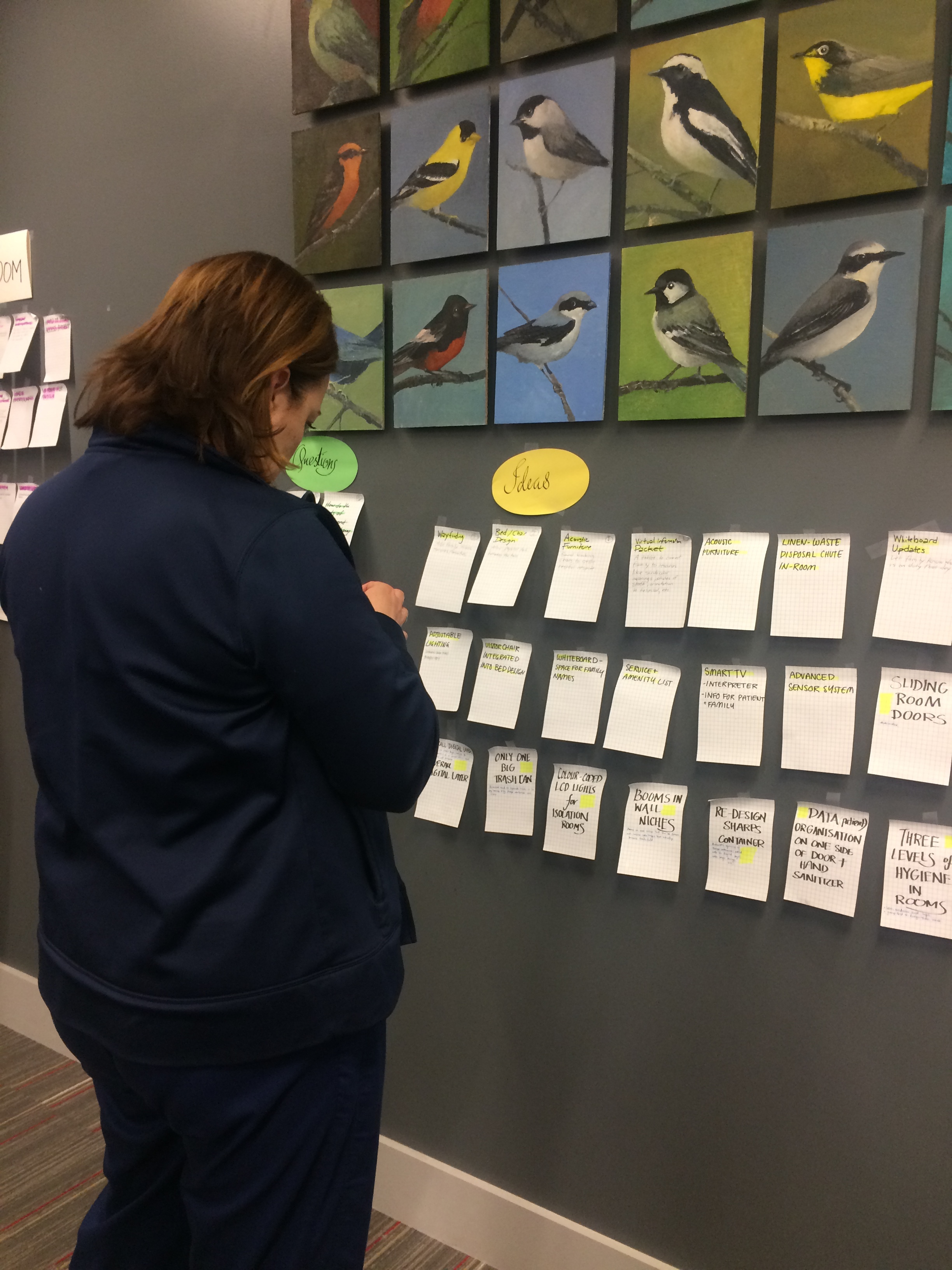
In the second workshop, the working points, pain points, and proposed new ideas were jotted down on large sticky notes for each of the four groups. The teams were shuffled to have members from each of the four main layers. In this process, we explored three streamlined topics: unit, room, and patient/family experience. Each groups posted stickies on walls under 'working points', 'pain points', and 'new ideas'. Staff members and practitioners participated in the workshop by going around in the room and choosing four main points in each of those categories by sticking a sticker on the back of the notes. The notes that were most populated with stickers were identified as the highest in priority.
I was a part of the 'Room' team in this round of workshops and my teammates were Rose, Jason, Kelly, and Steve.
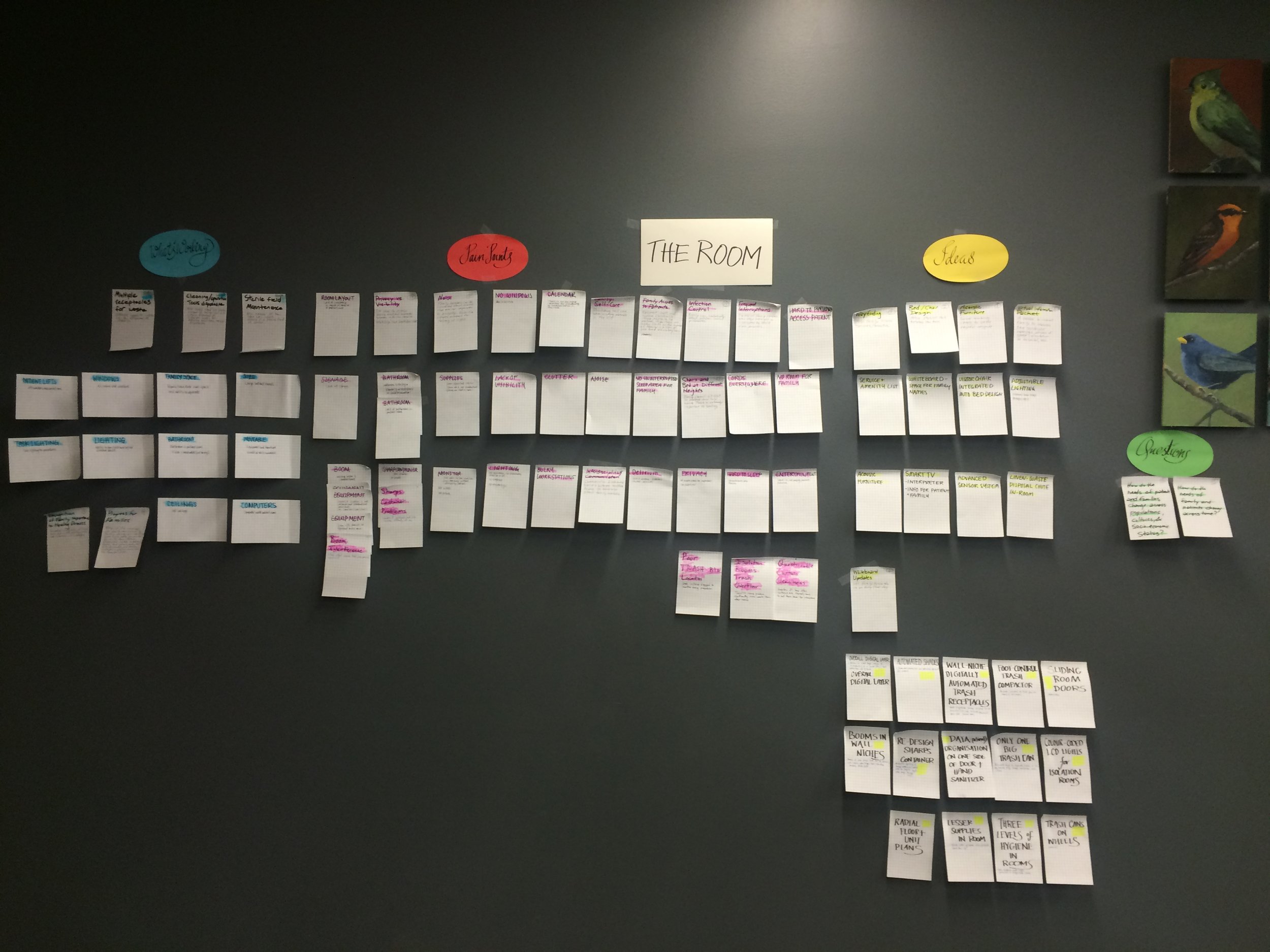
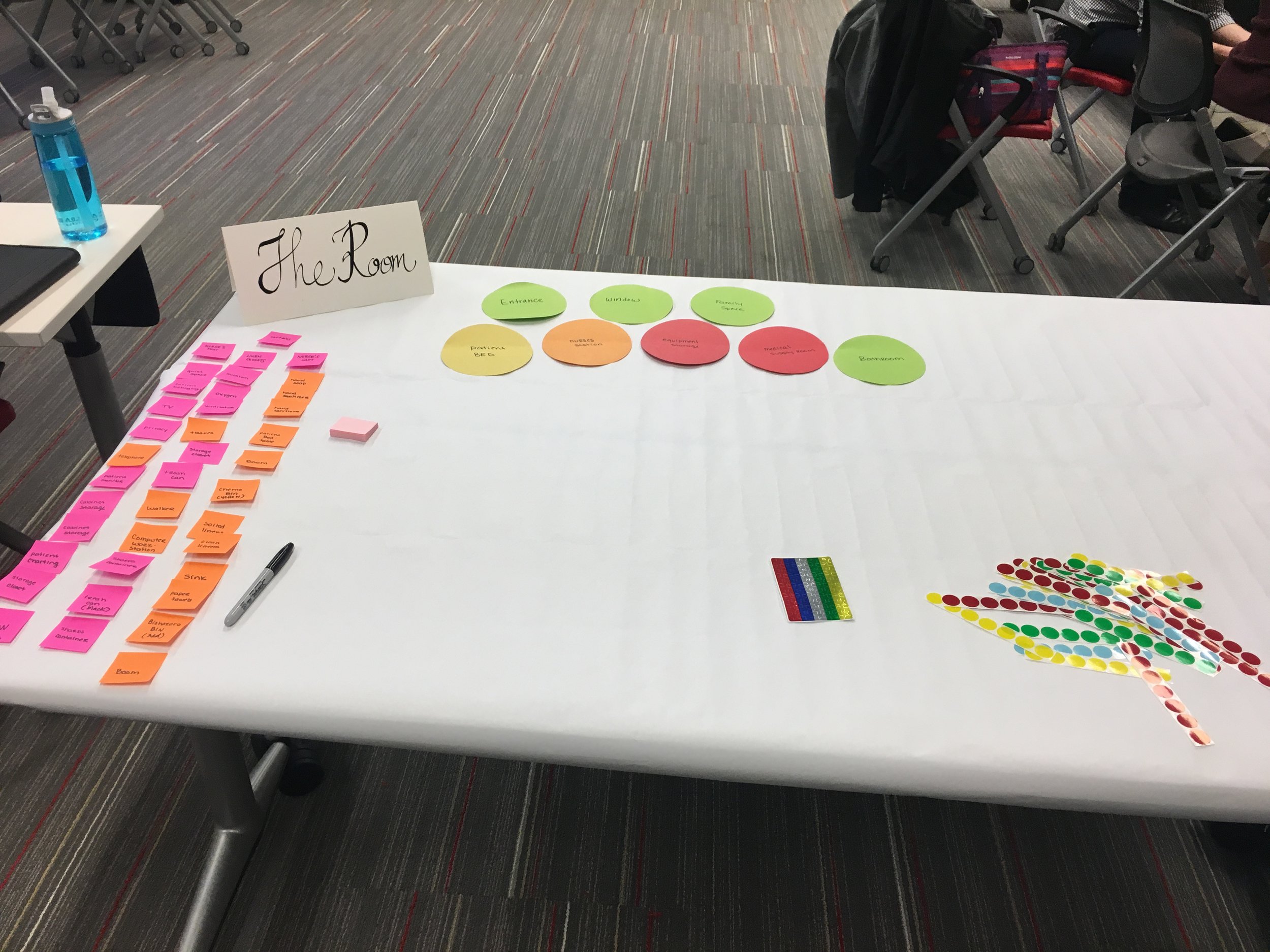
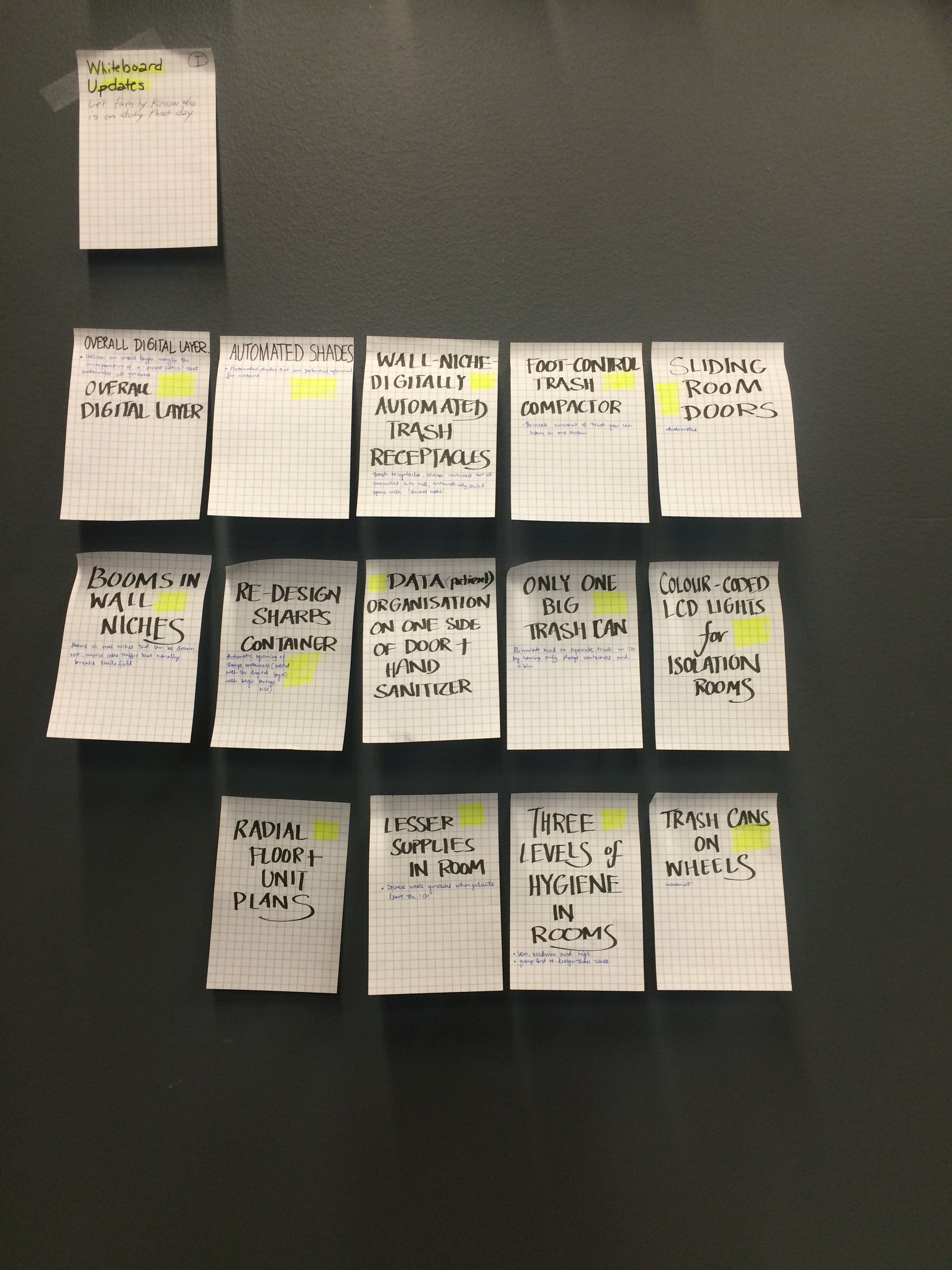
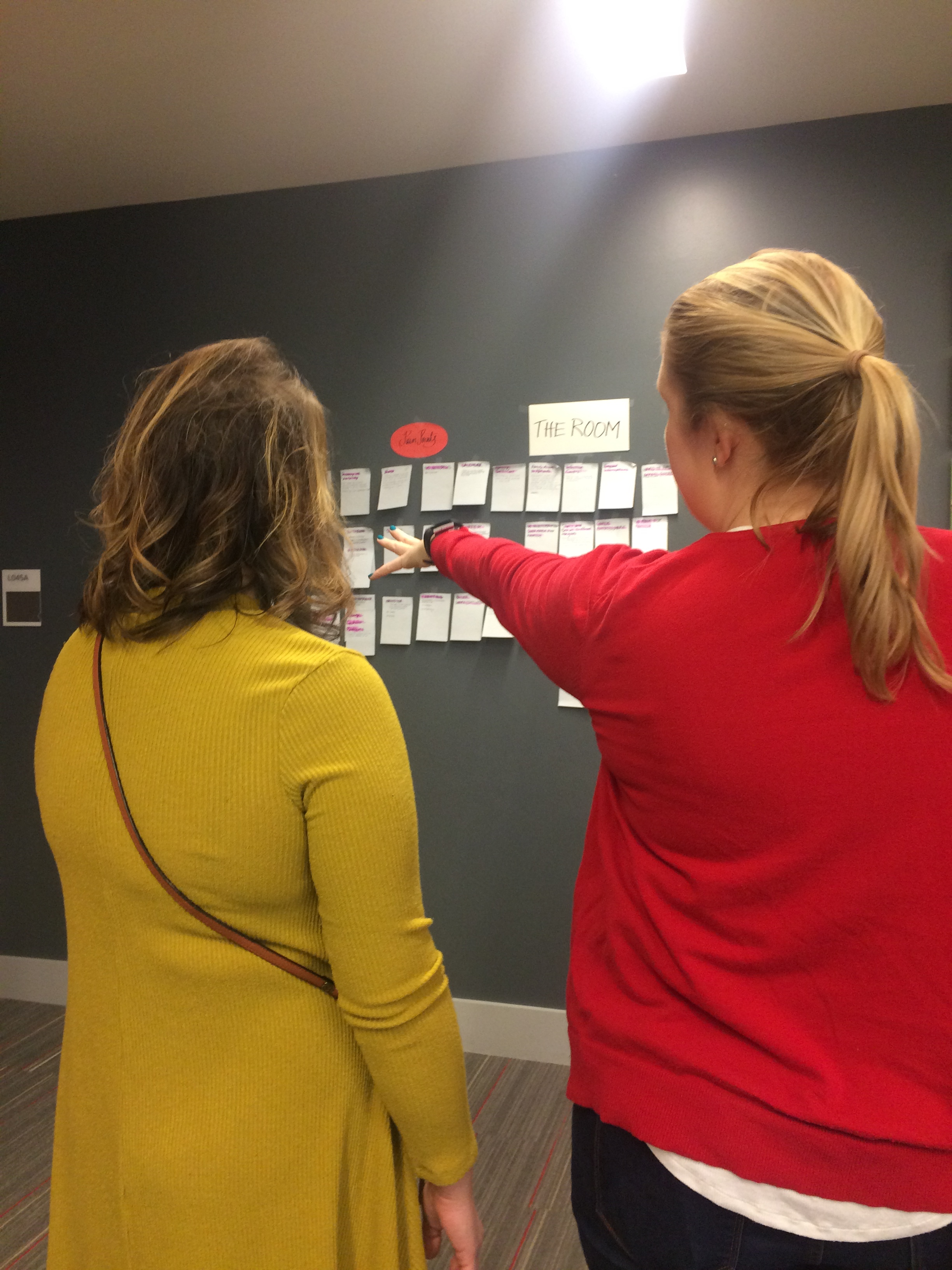
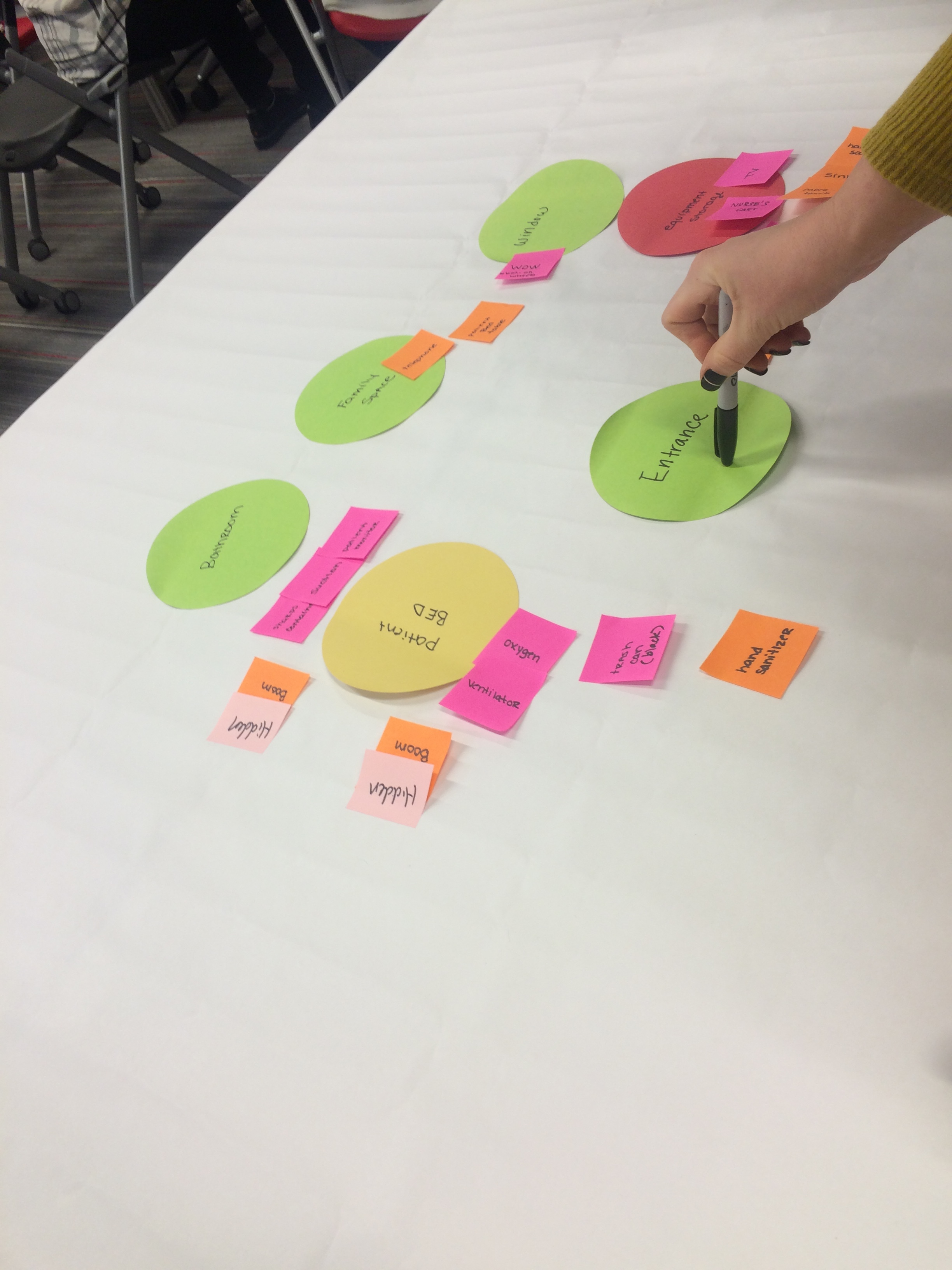
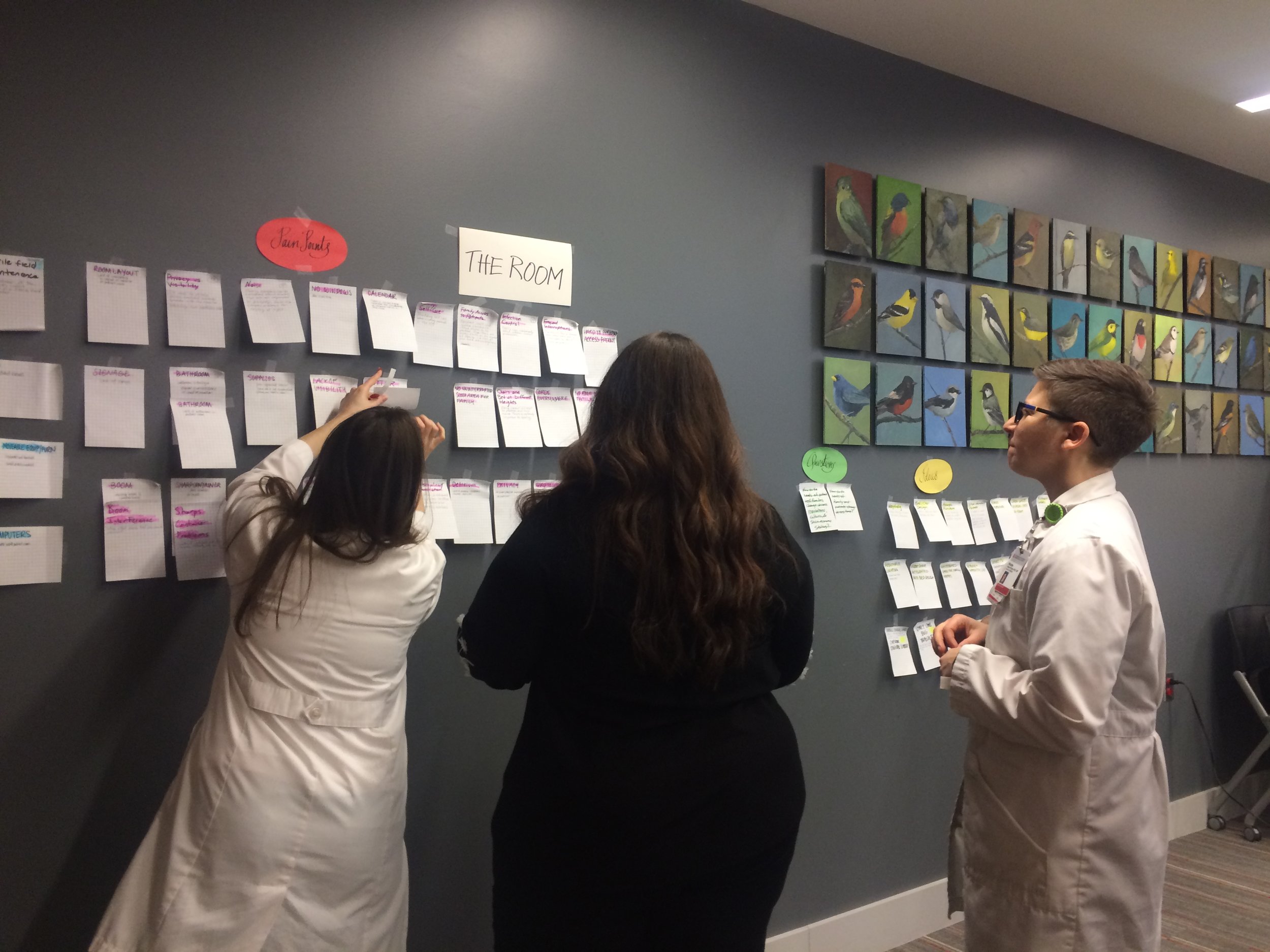
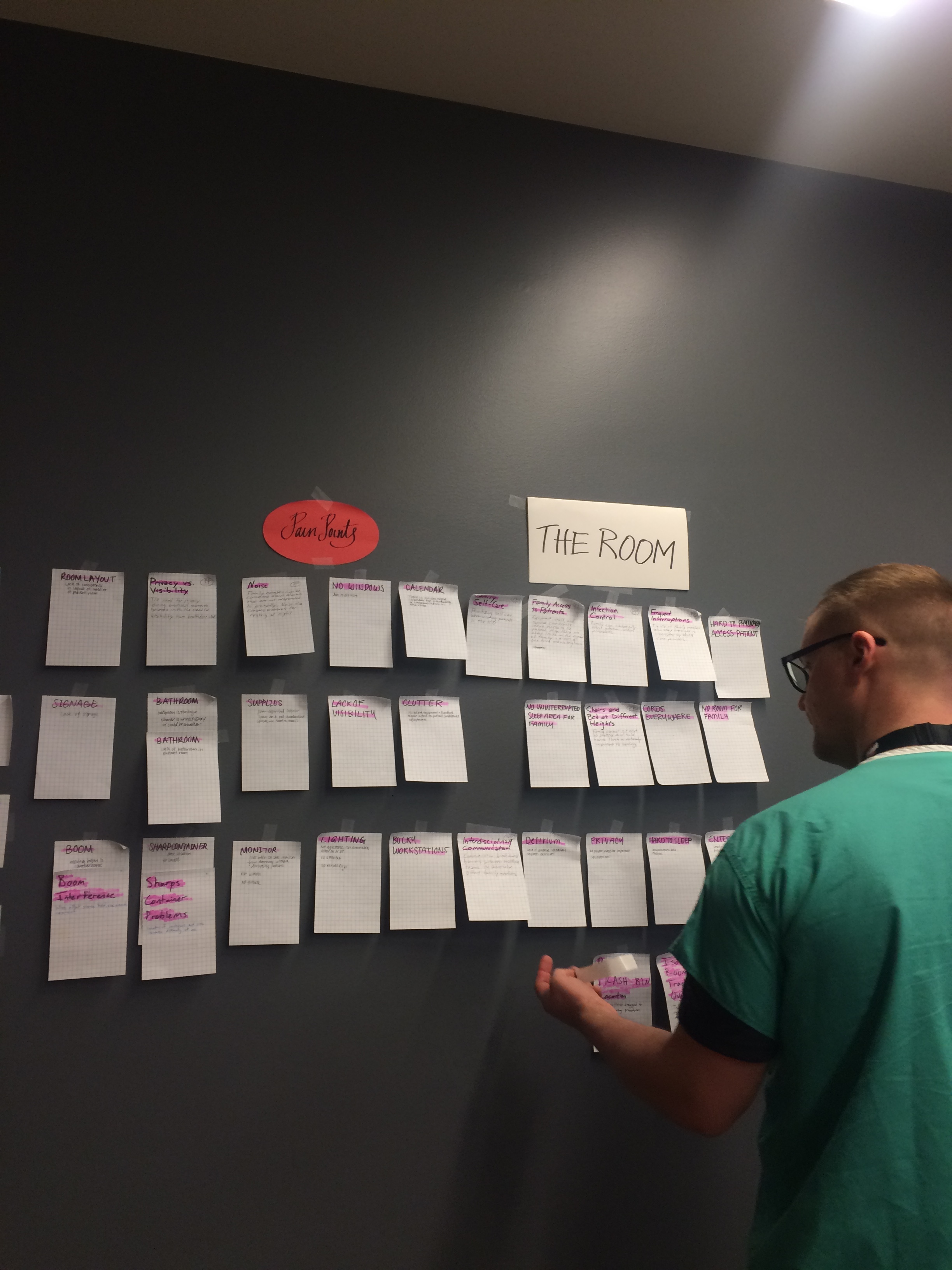
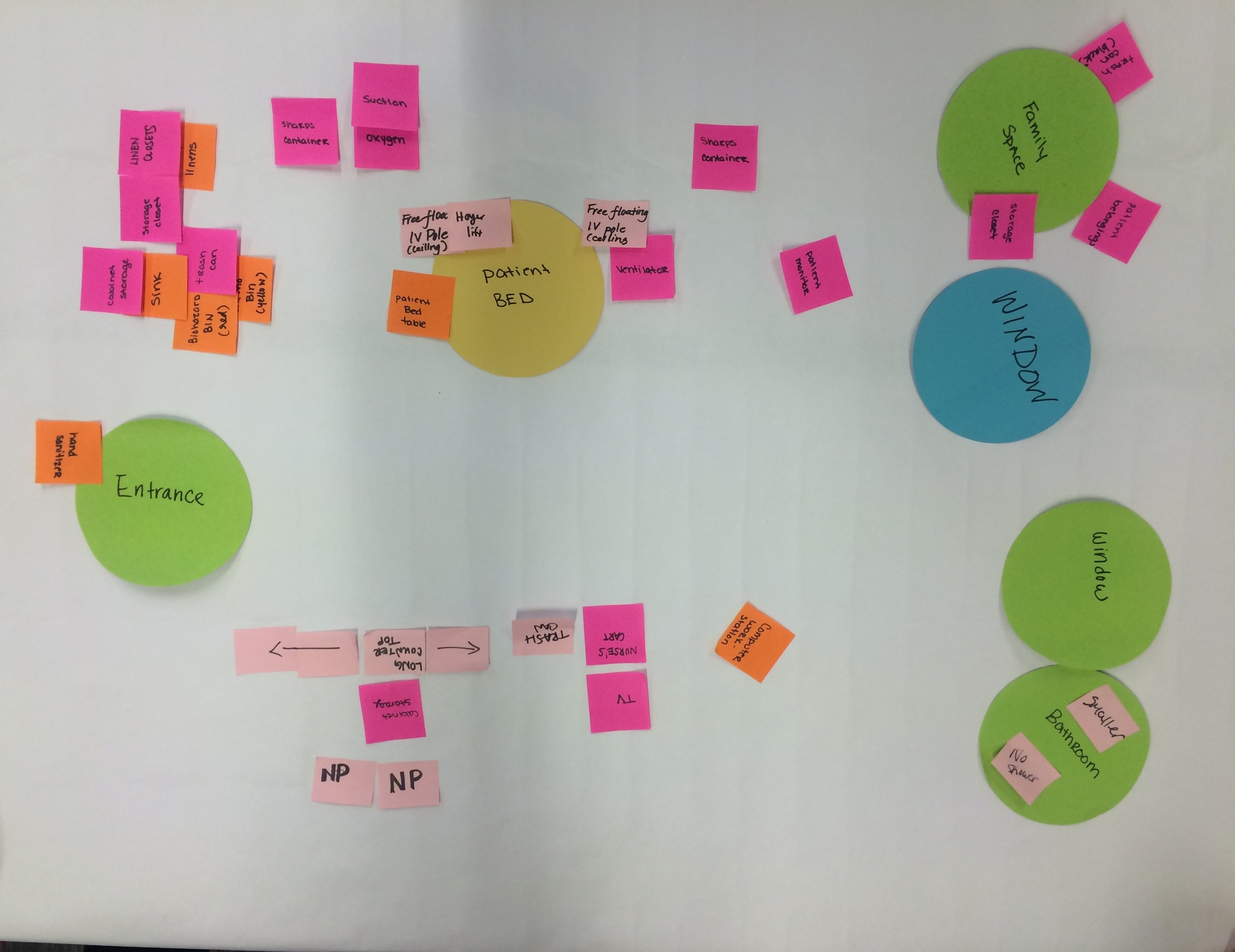
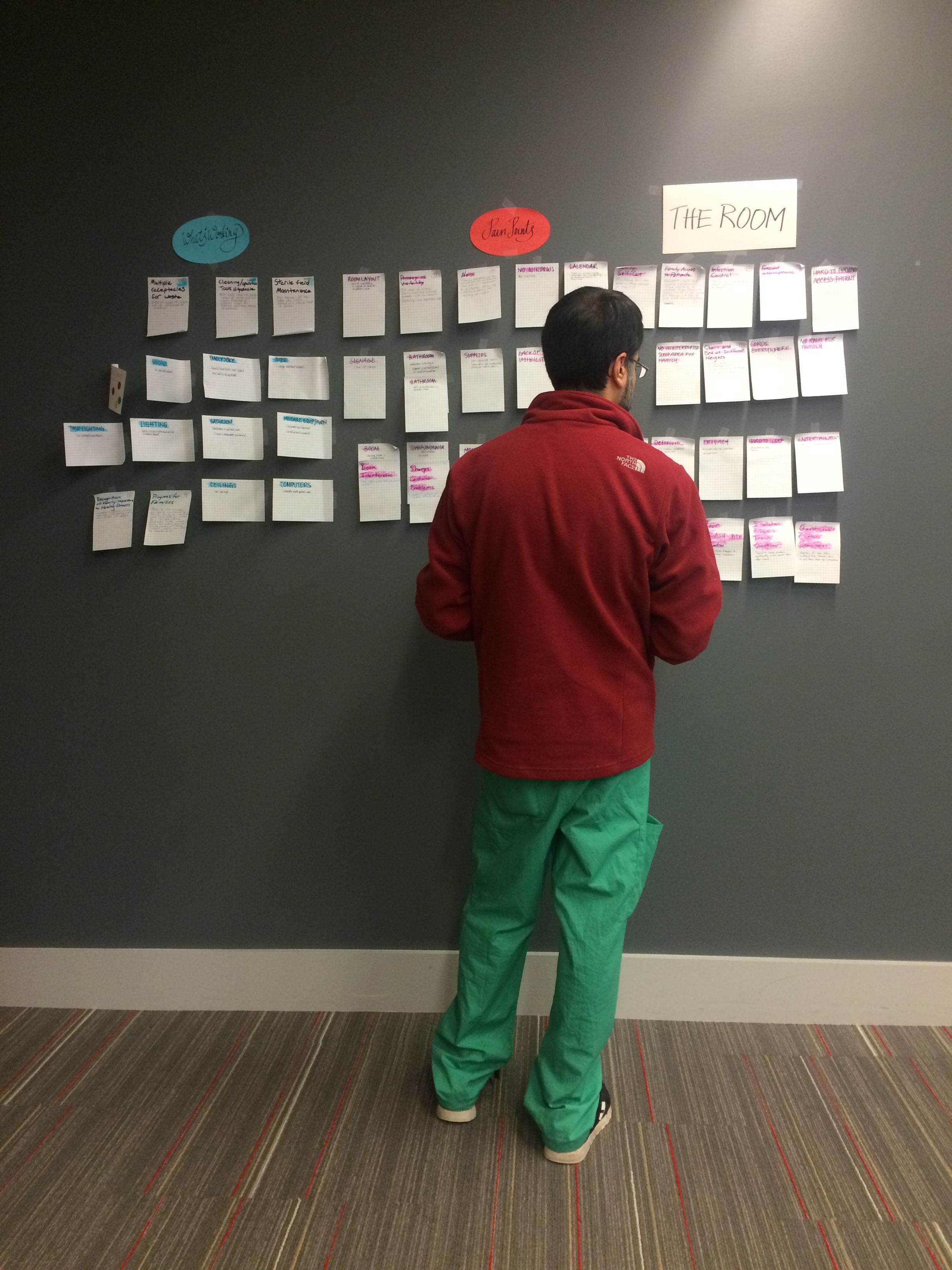

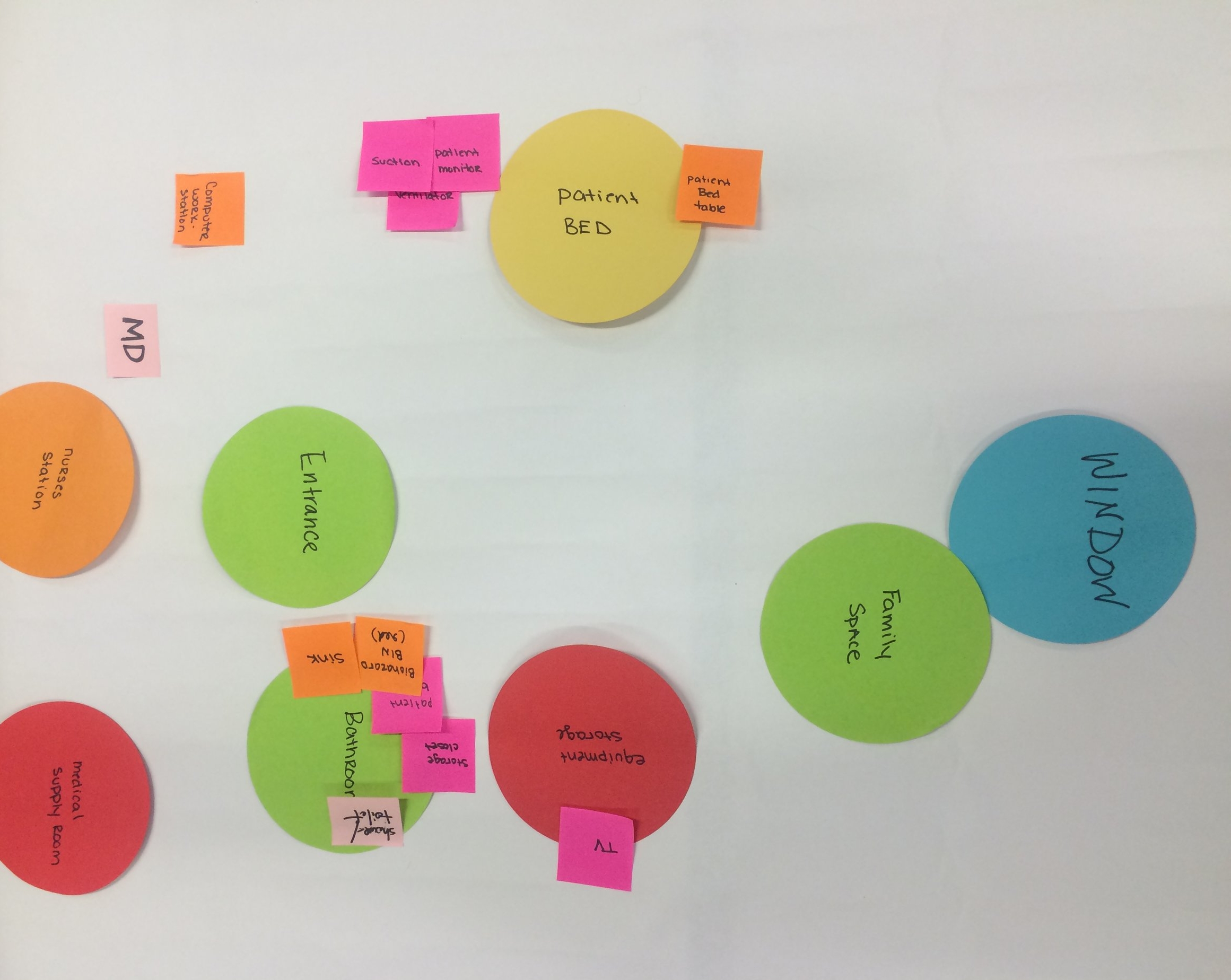
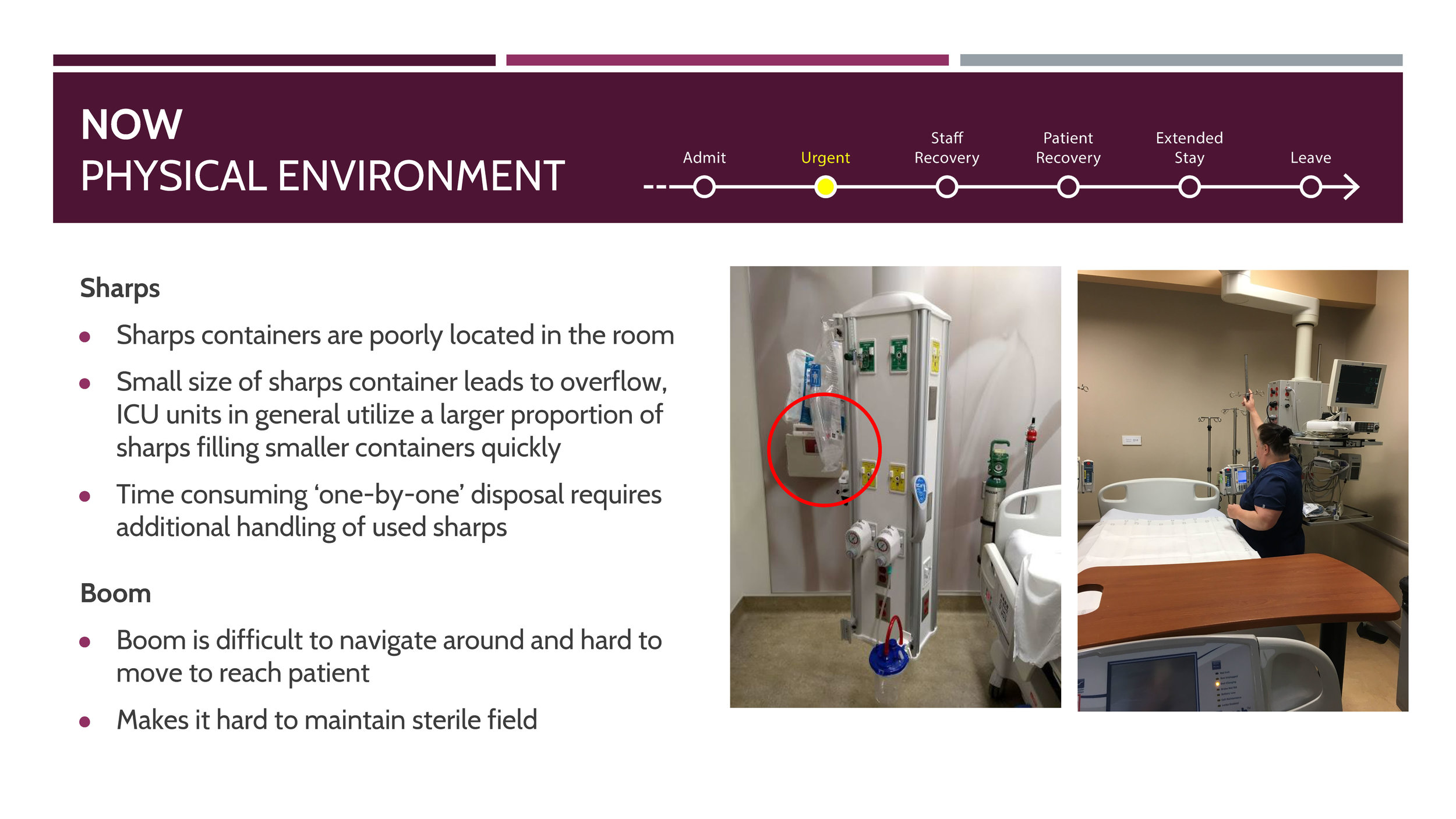
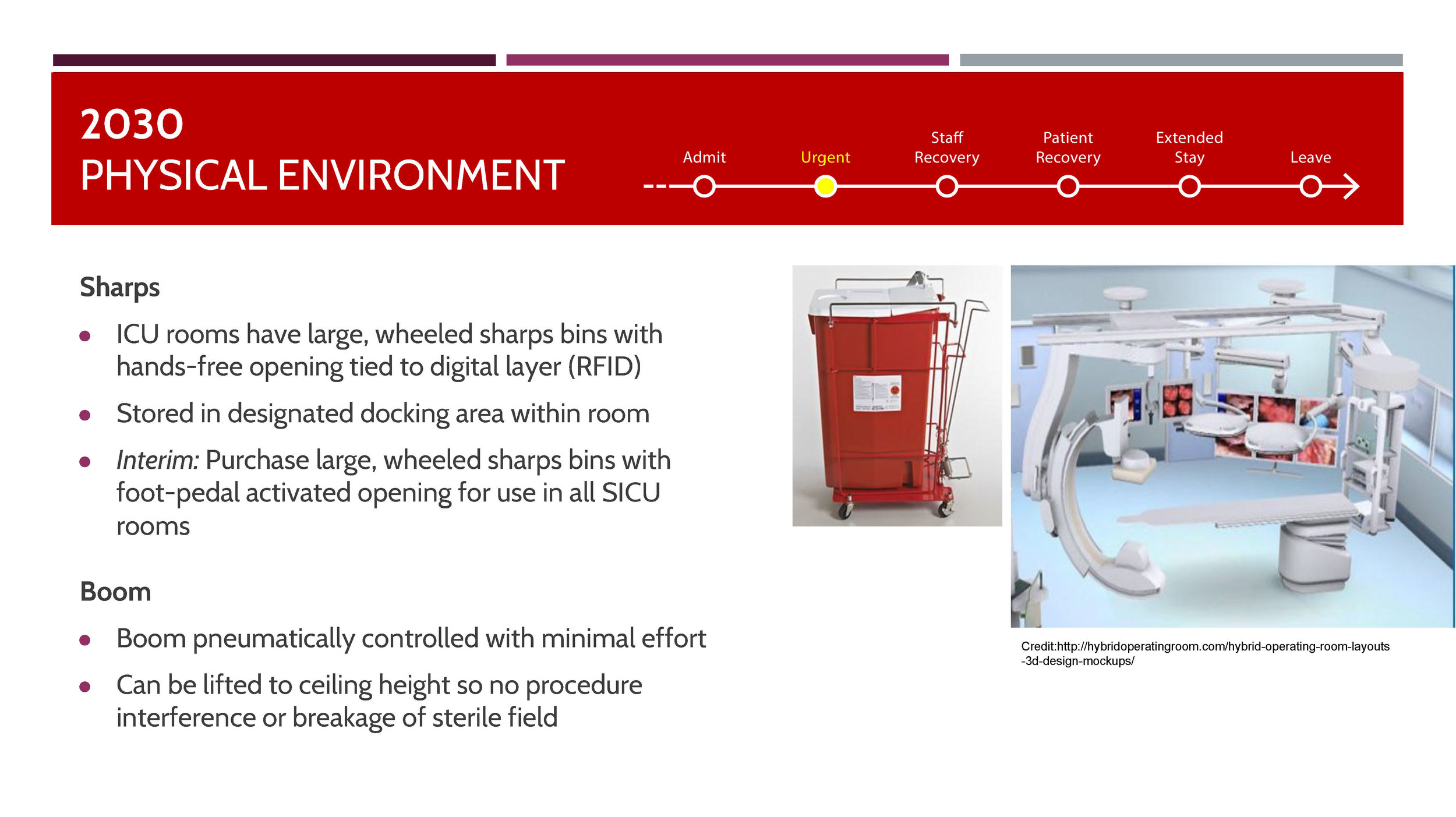
Along with the prioritization exercise, our team also conducted a mapping exercise using sticky notes and sharpies and asked the staff to depict their ideal ICU surgical unit and room. These were later organized using Excel and was analyzed for patterns and repeated points of interest. We also conducted a separate workshop on the use of sharps and booms, and their potential future development for ease of use.
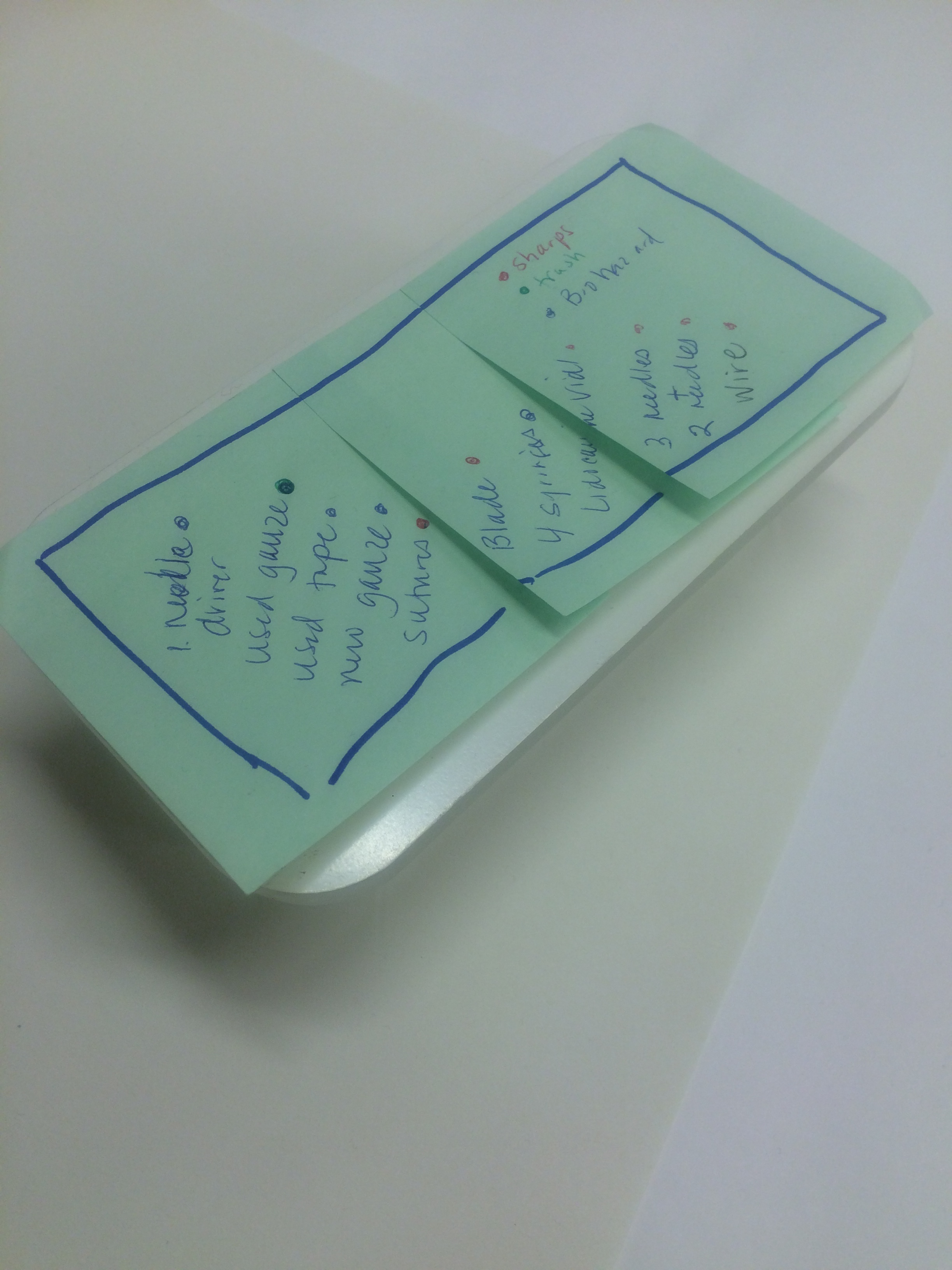
The toolkit for 'Redesigning of the Sharps Container' workshop
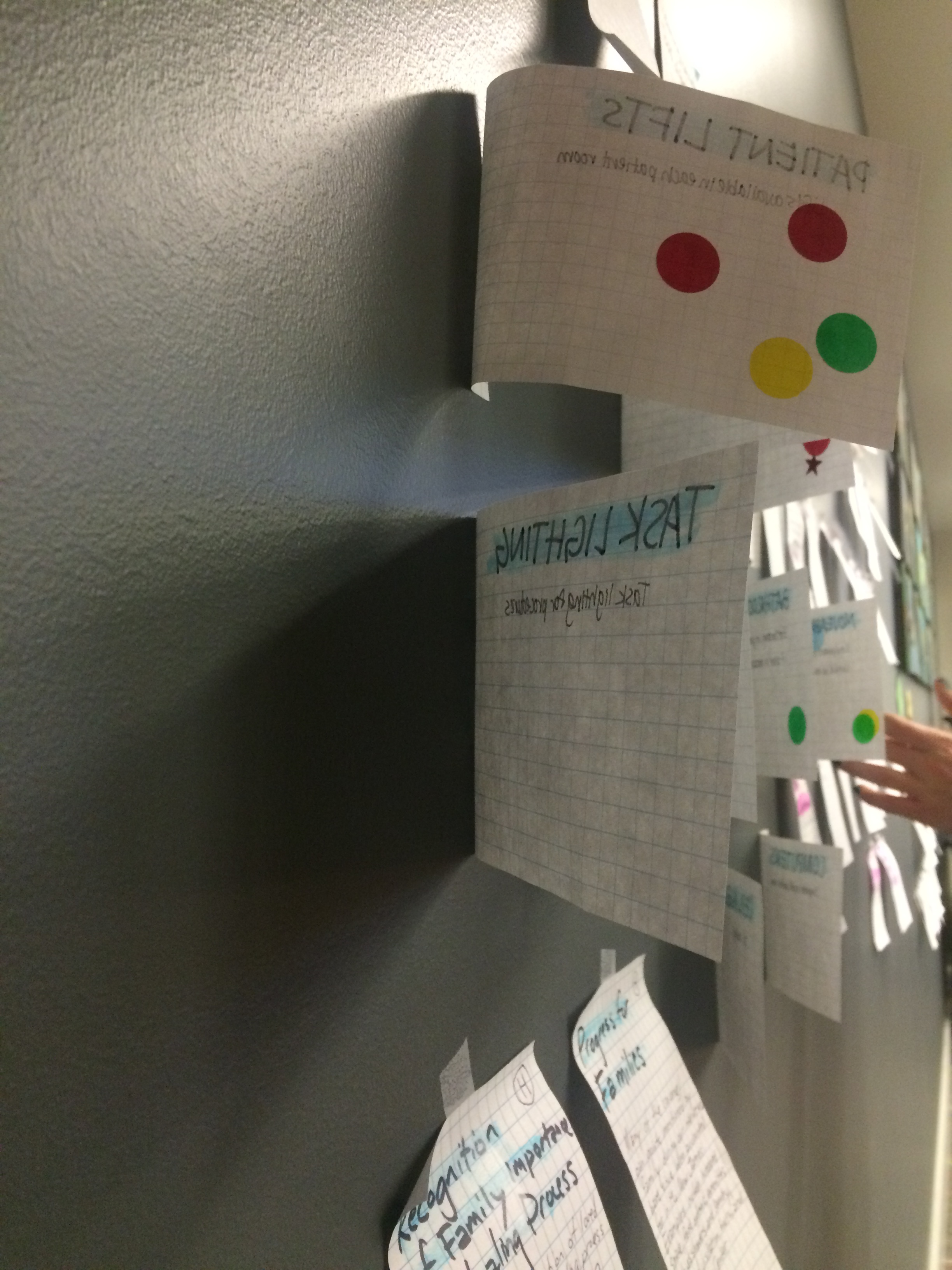
Medical healthcare practitioners went through a small exercise where they remapped their ideal ICU room solely concentrating on the positions of sharps containers and their designated spots using the dolls and building lego blocks. They also went through a series of sharps container options and picked their best and worst picks which were later used in our analysis process. The sticky notes from the workshop-2 were taken on into the next classroom discussion where we mapped them across each topic.
Phase 2 | Workshop 3 : Exploring Future Scenarios of Use
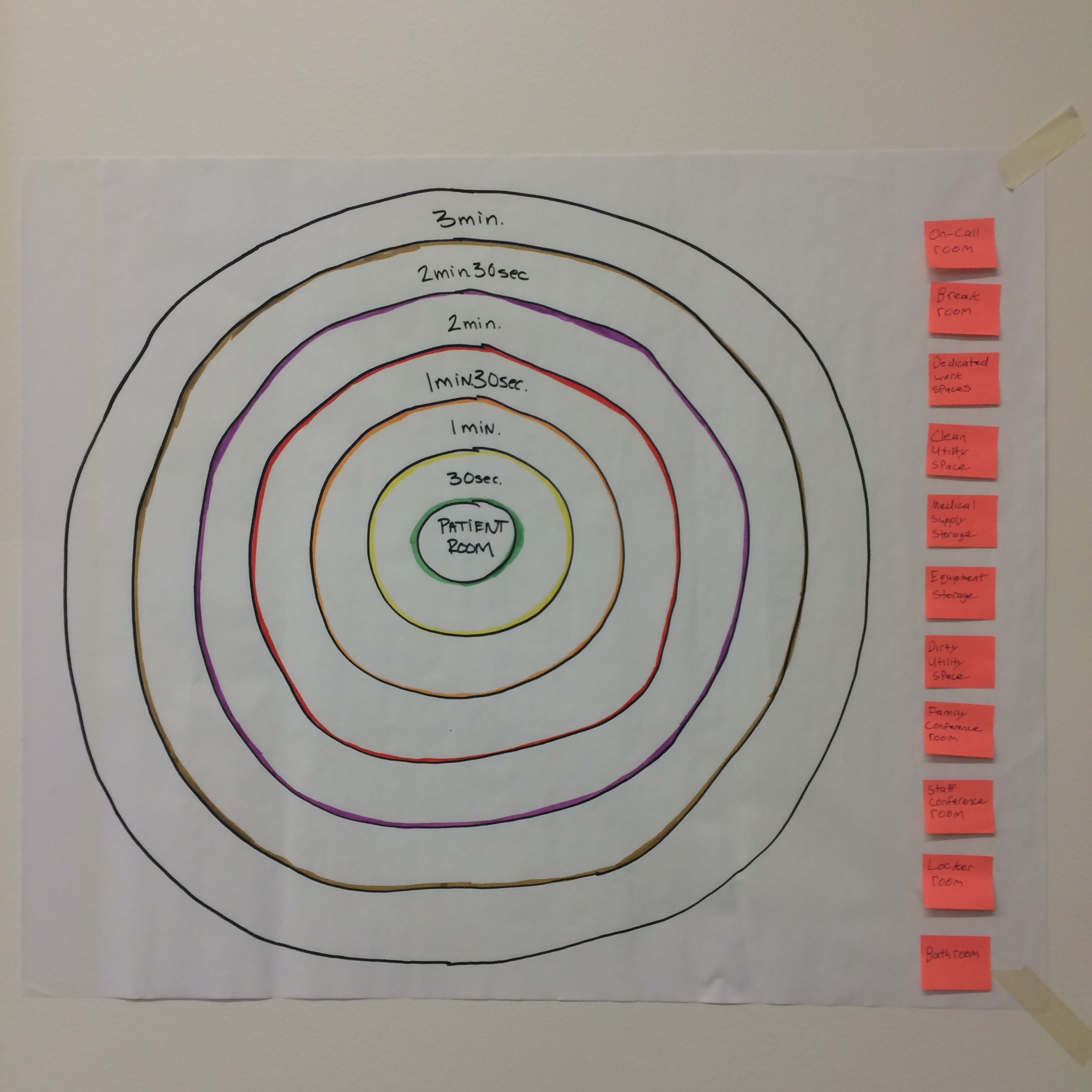
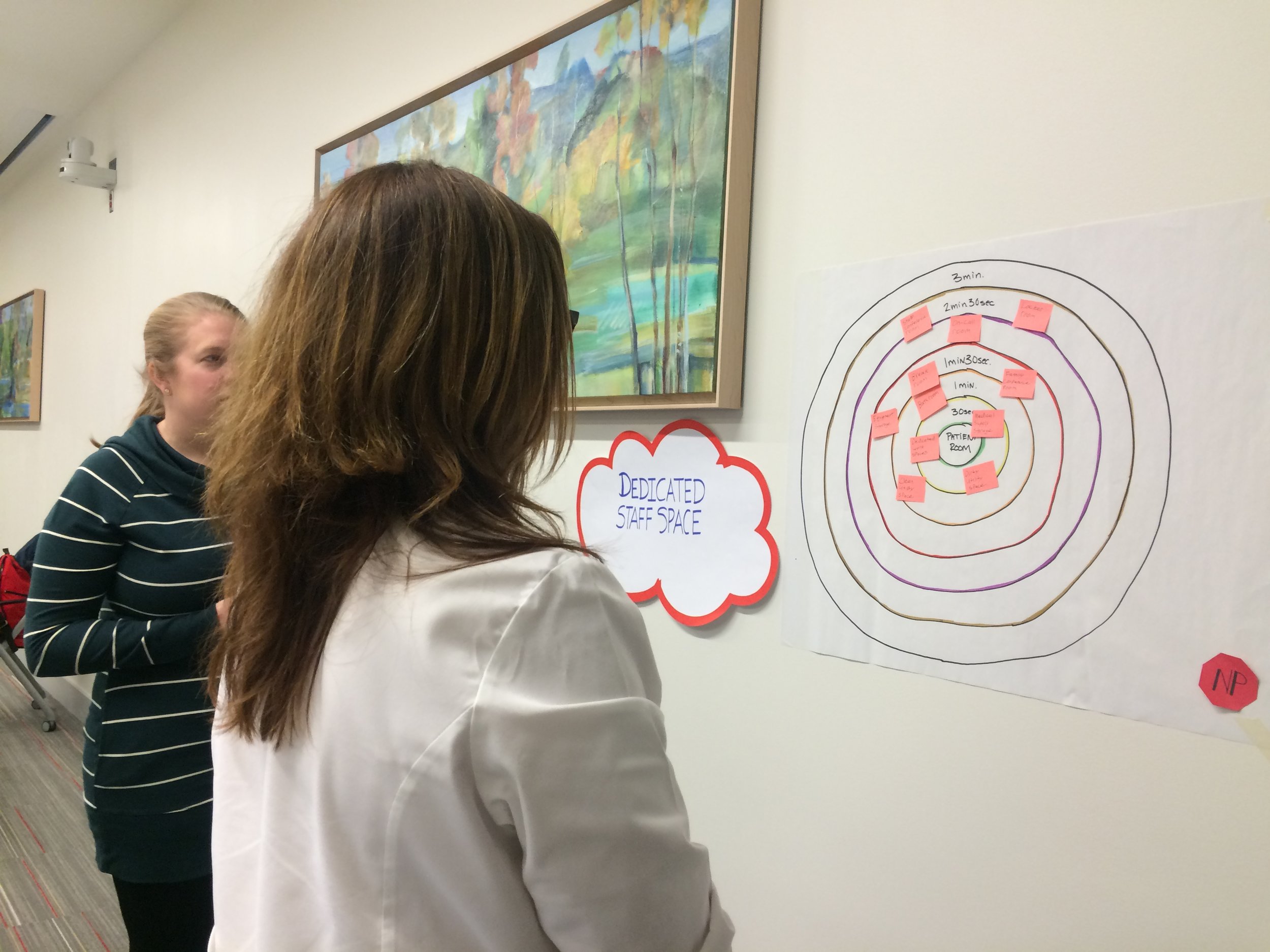
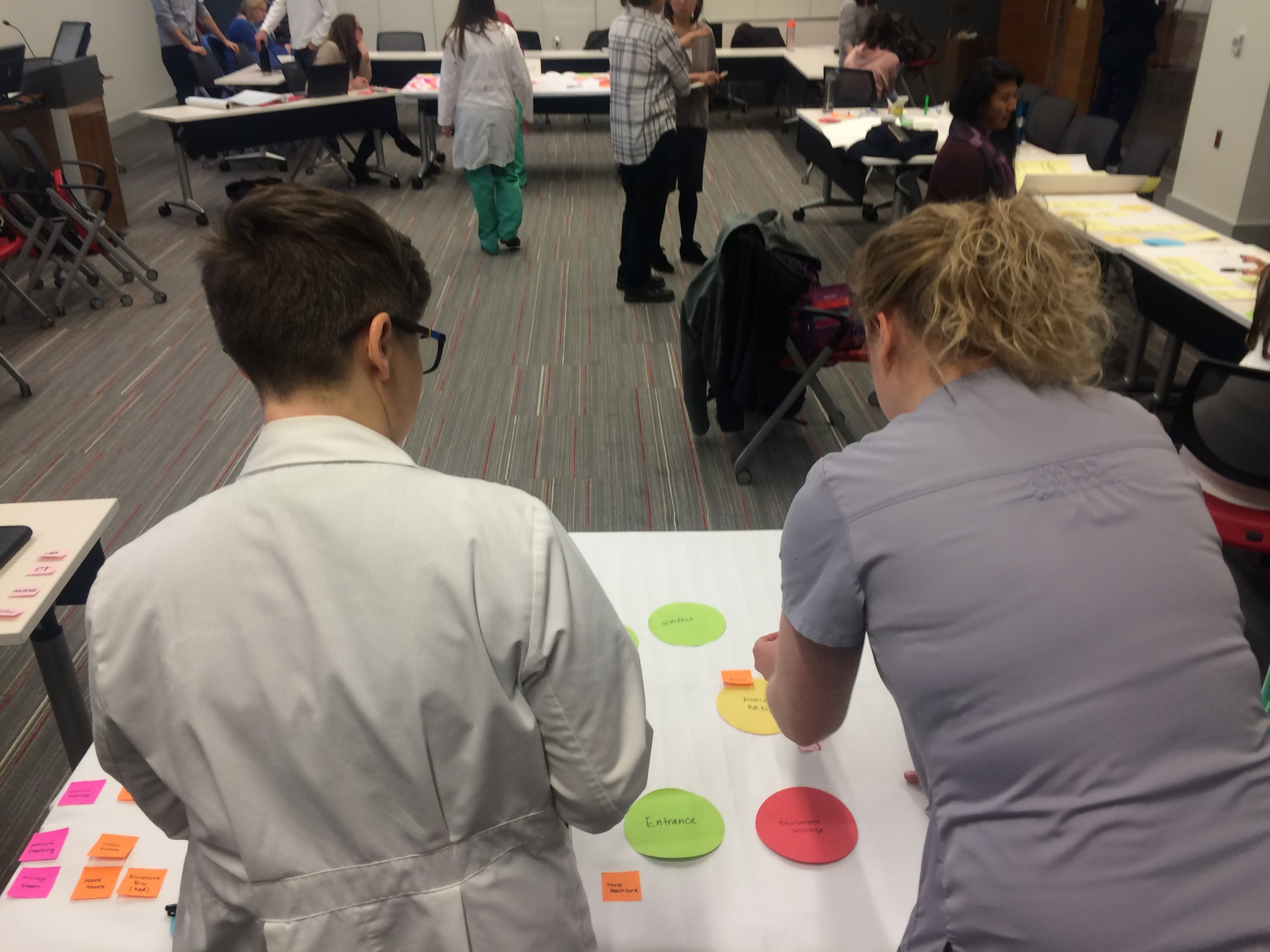
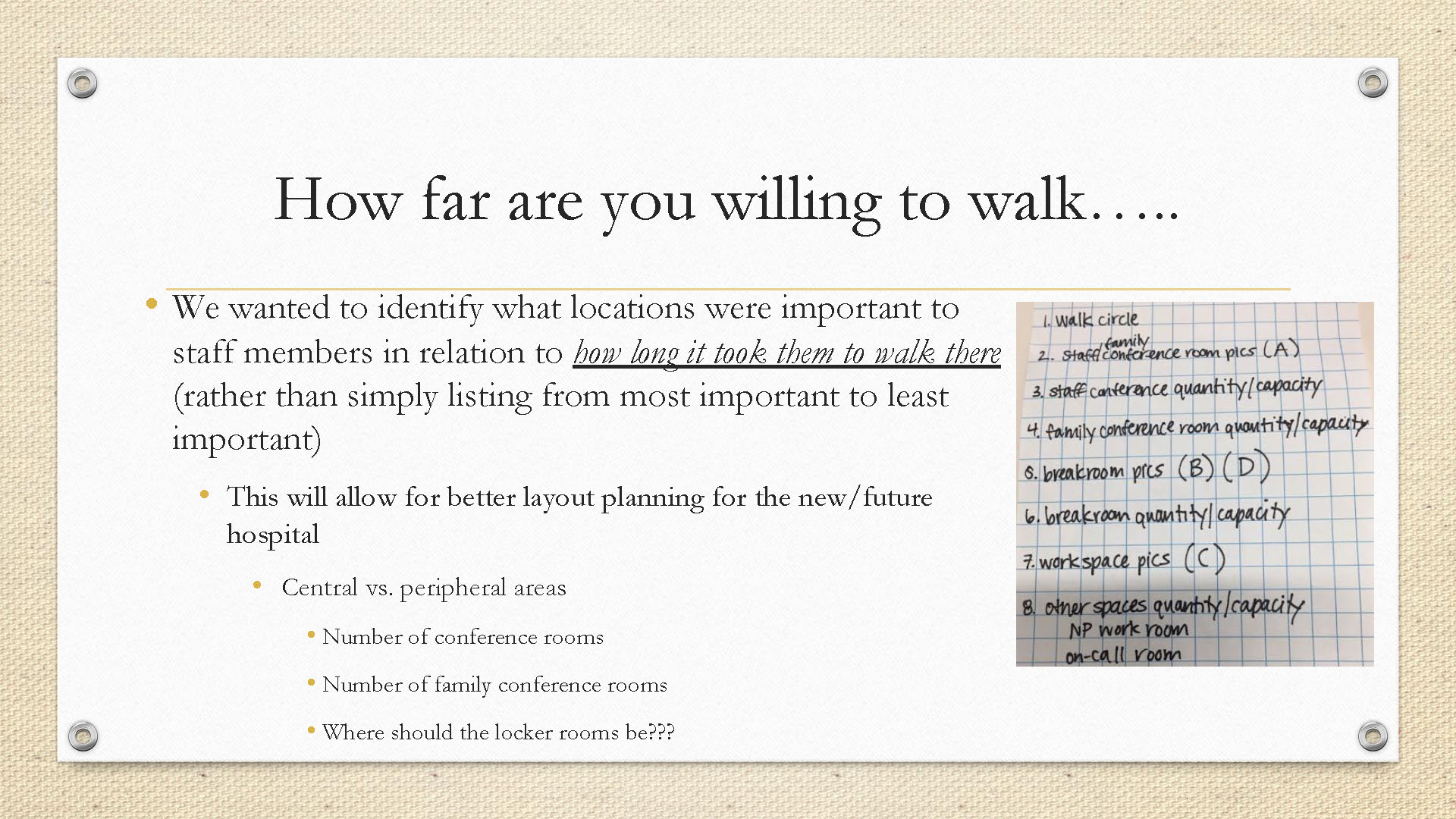
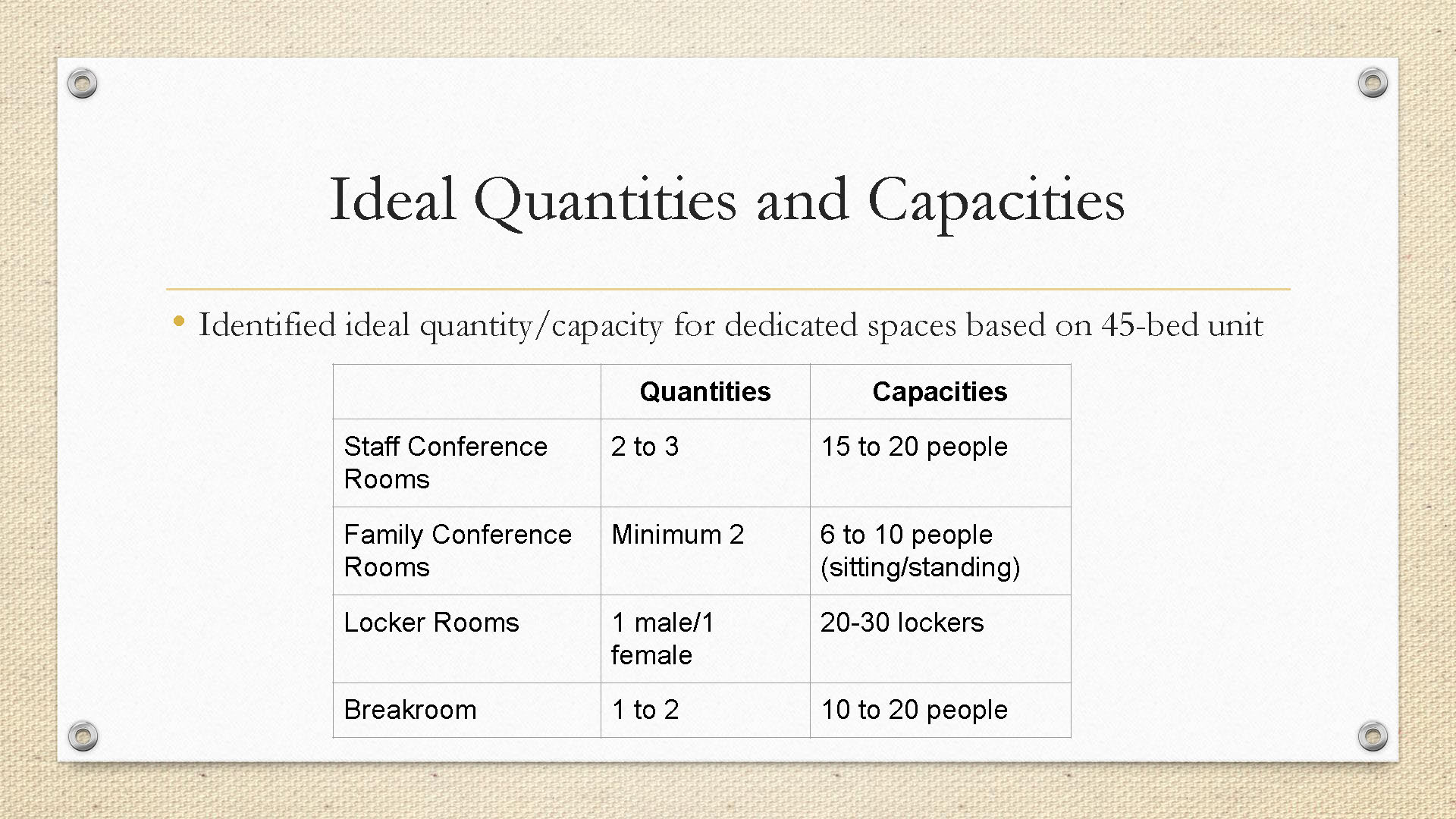
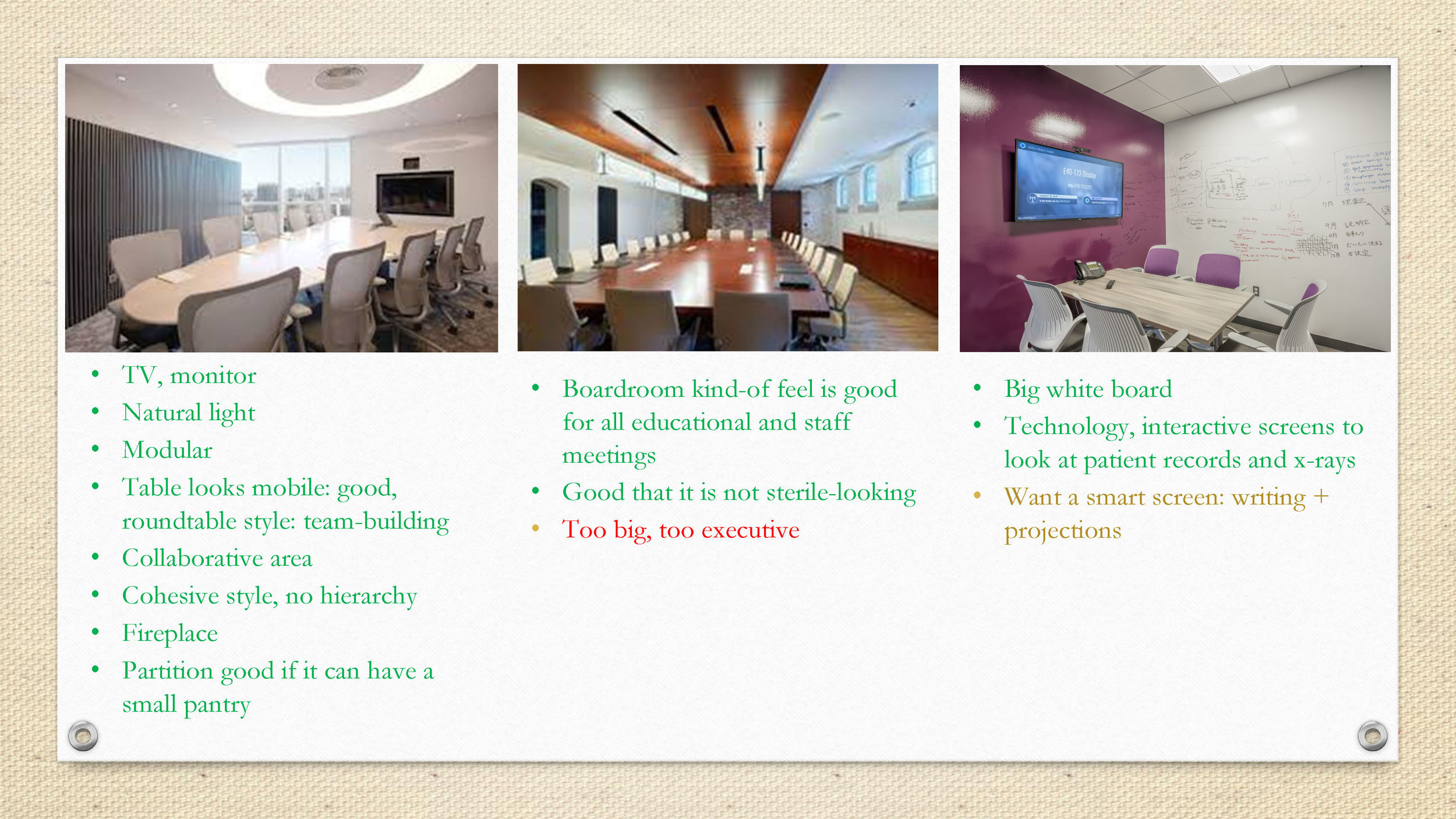
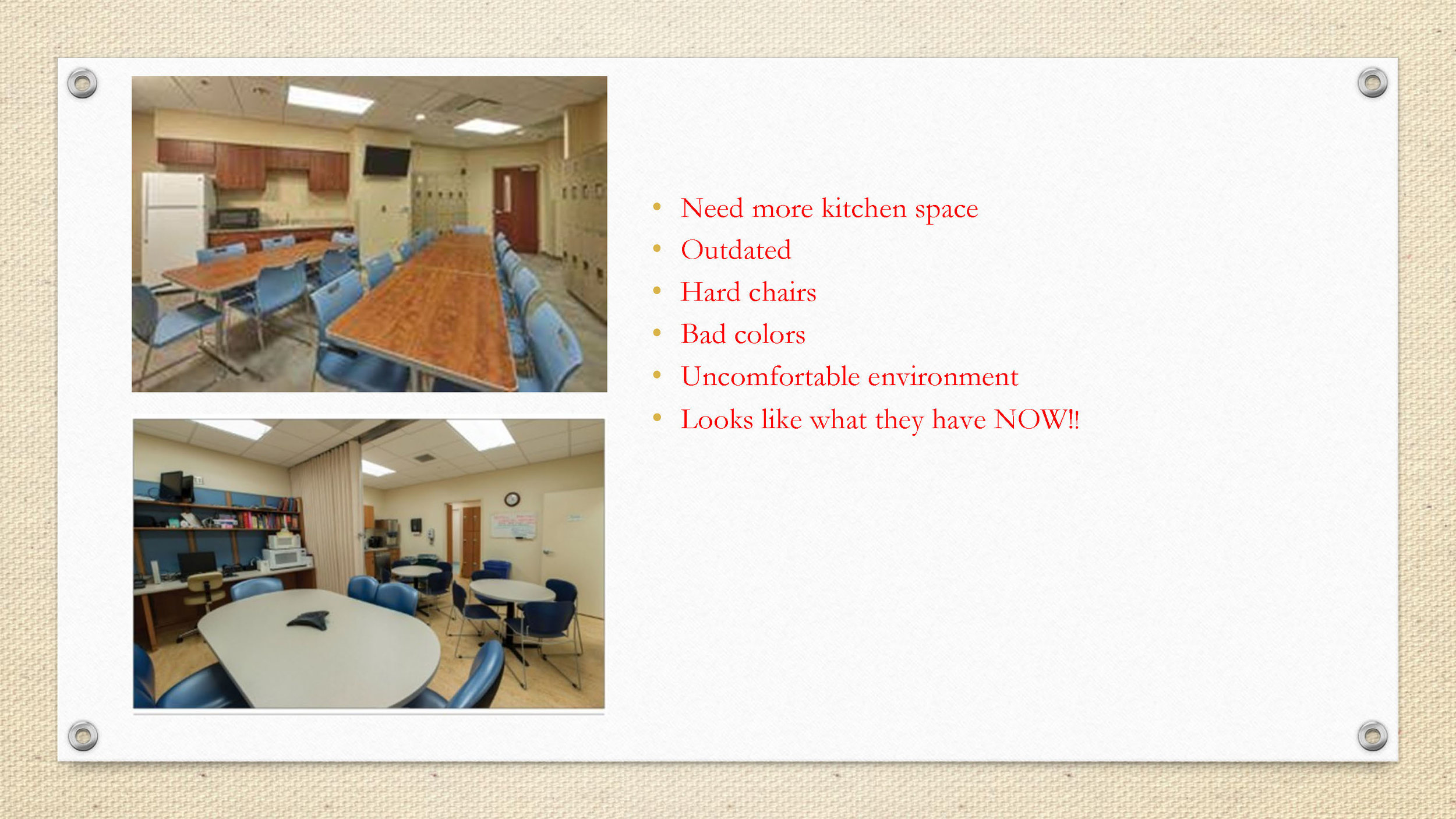
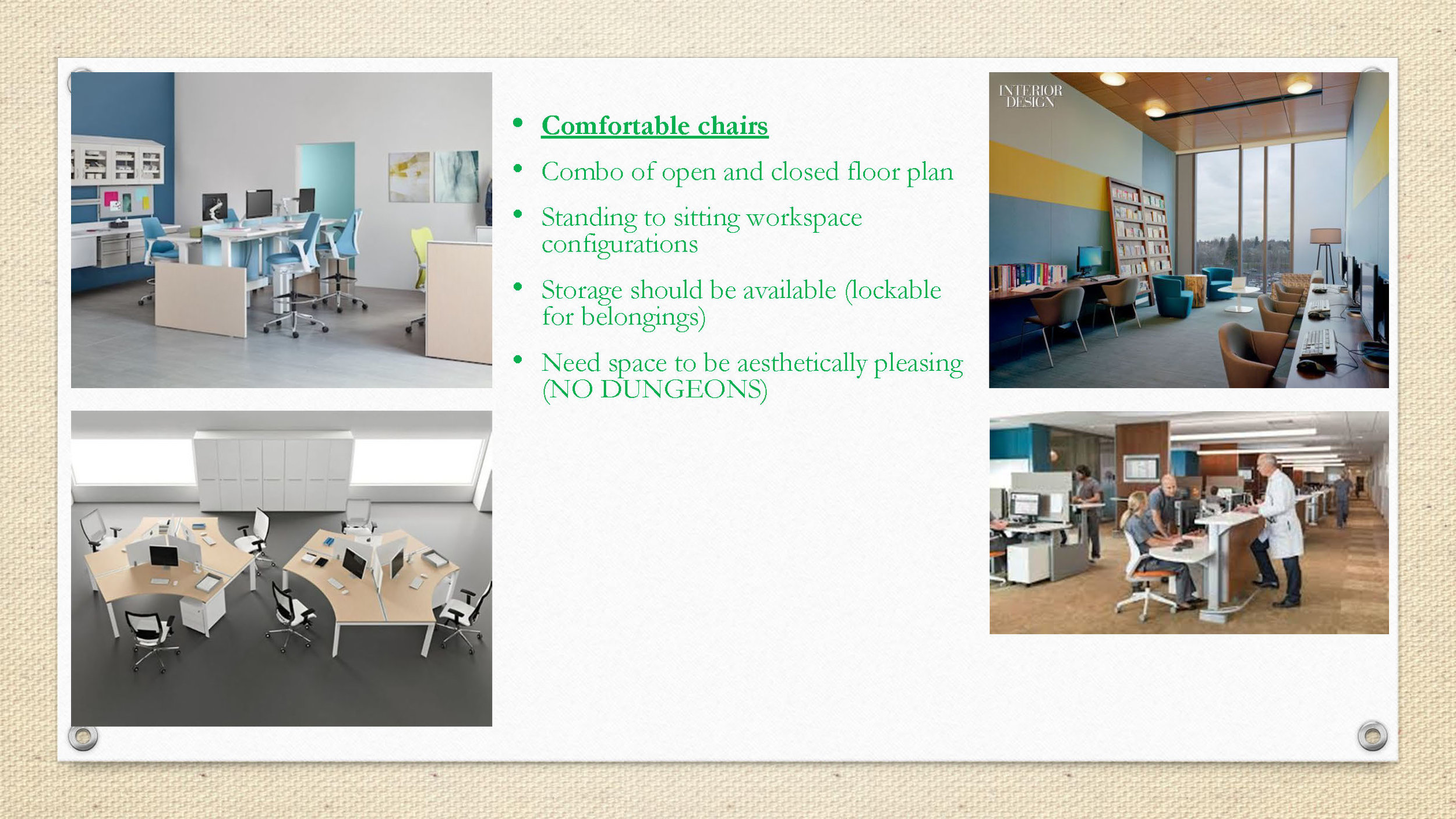
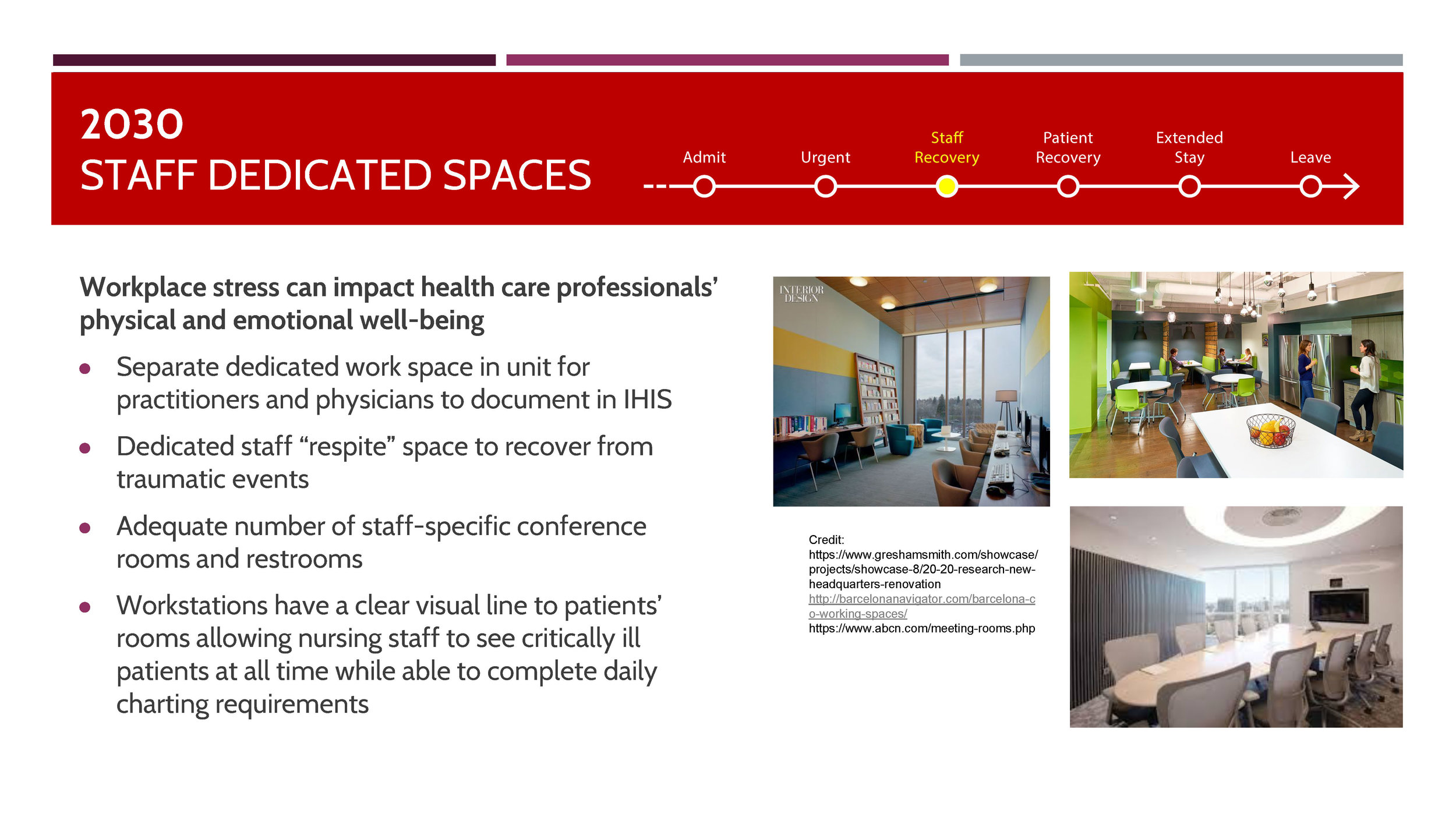
This workshop was geared towards the future use and development of systems, products, and plans for the upcoming surgical units. Teams were regrouped once again, and 8 main topics were established for further development based on the findings from the process: booms, sharps containers, staff communication, patient/family experiences, lighting, linear vs. pod layouts, doorways and visibility, and dedicated staff spaces. The third round of workshops involved the staff engaging in exploring future scenarios of use based on information collected so far from generative sessions. I was a part of the 'dedicated staff spaces' team in this round of workshops along with Mike, Allison, and Kelly.
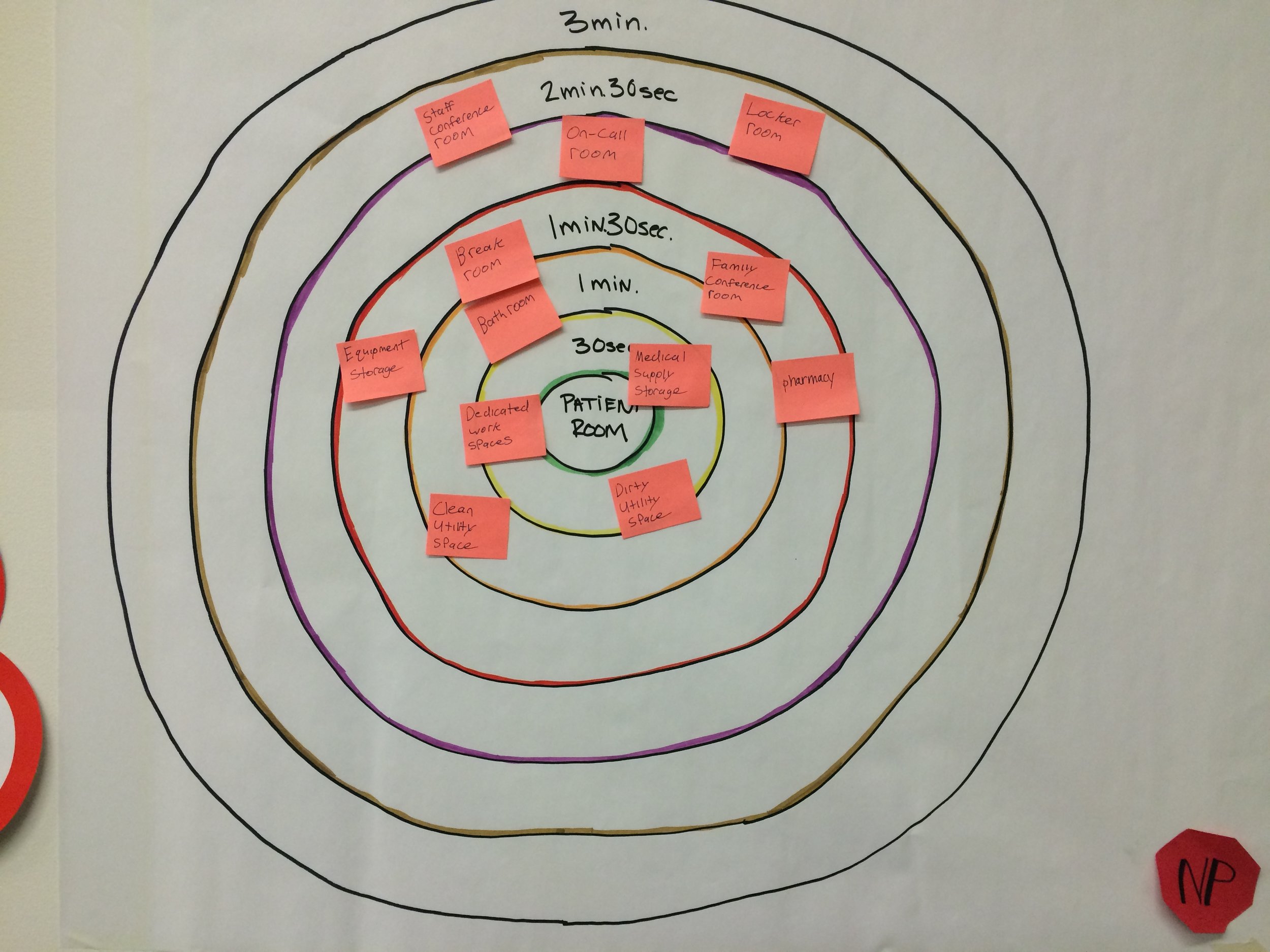
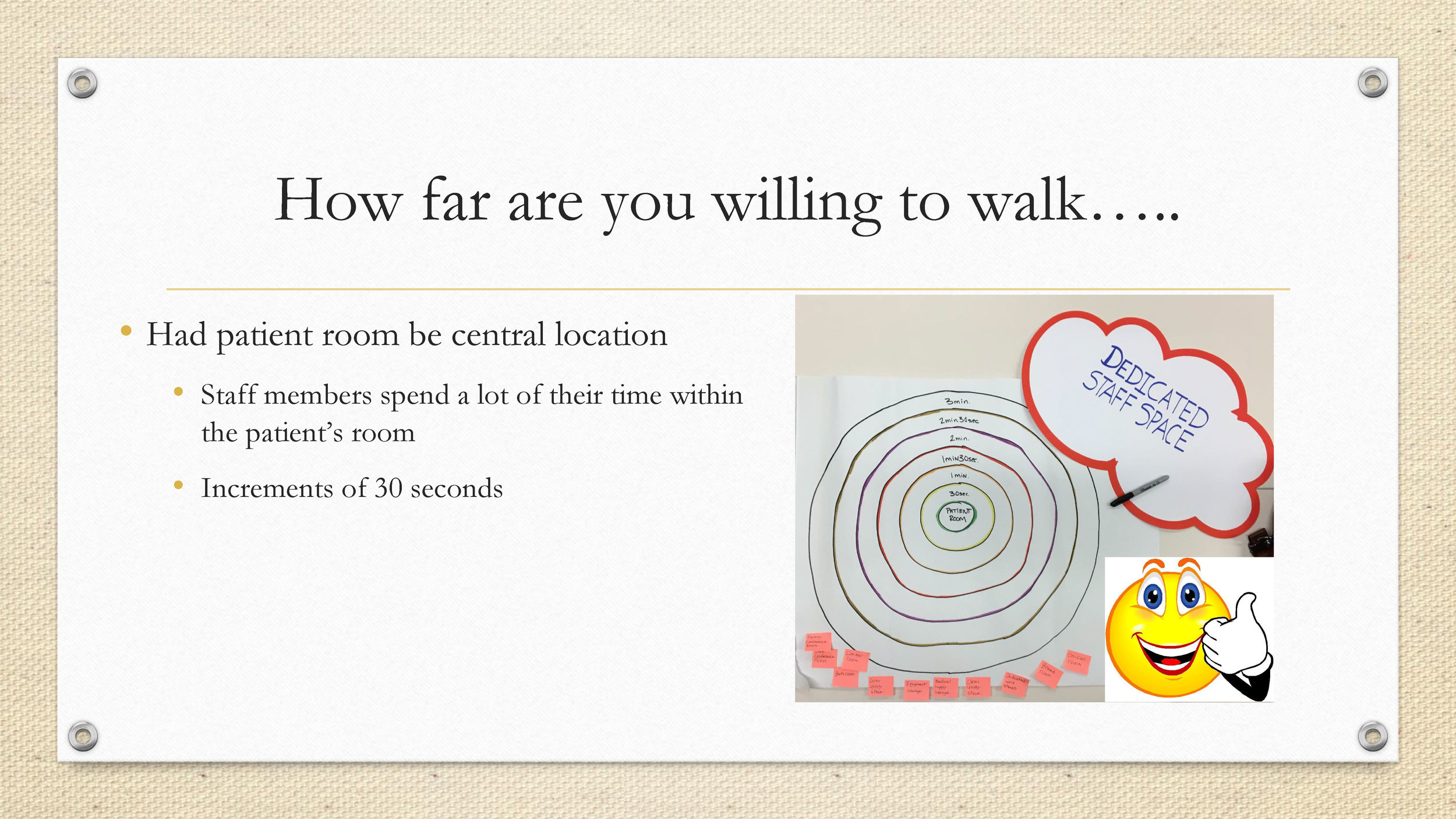
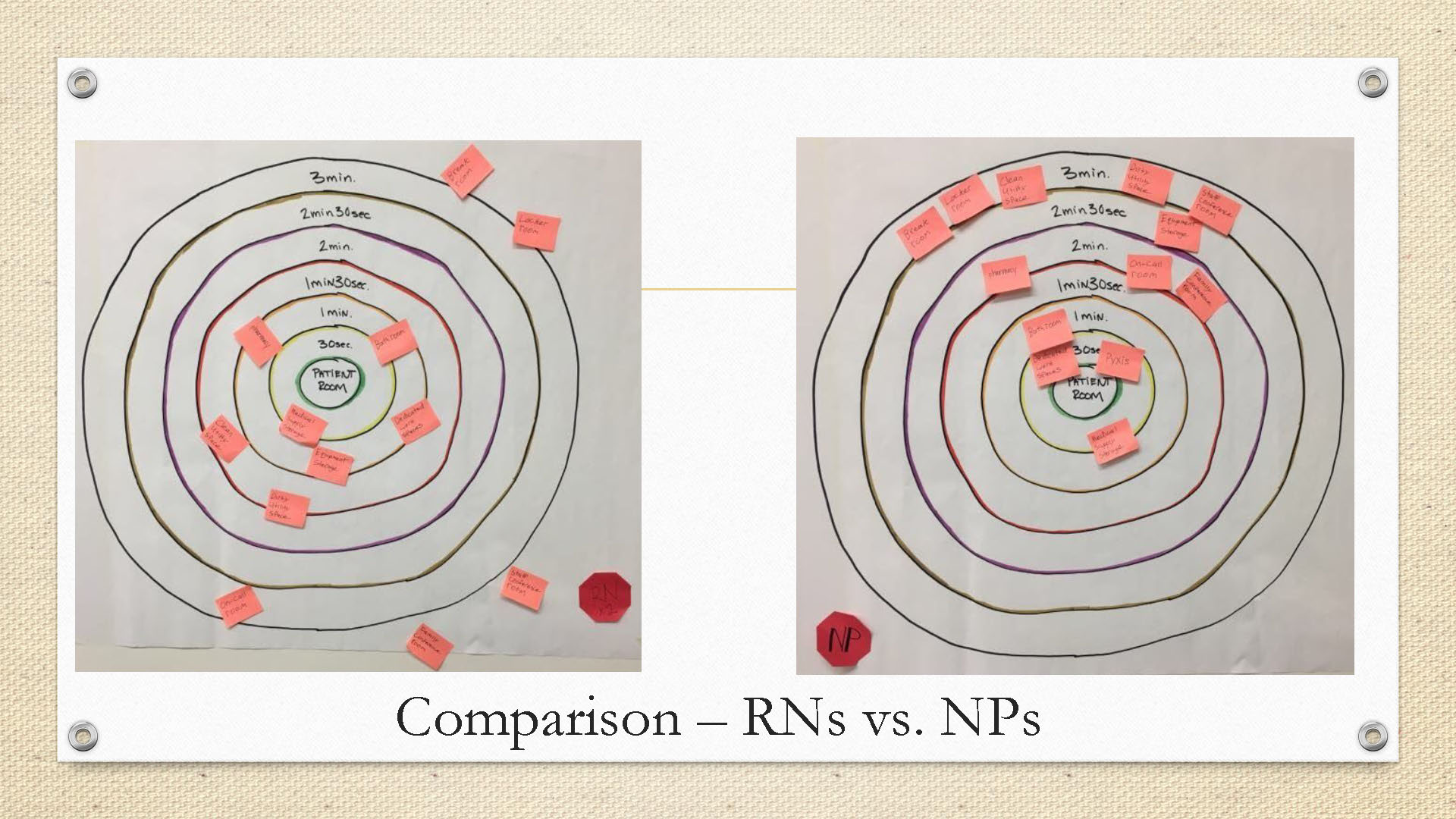
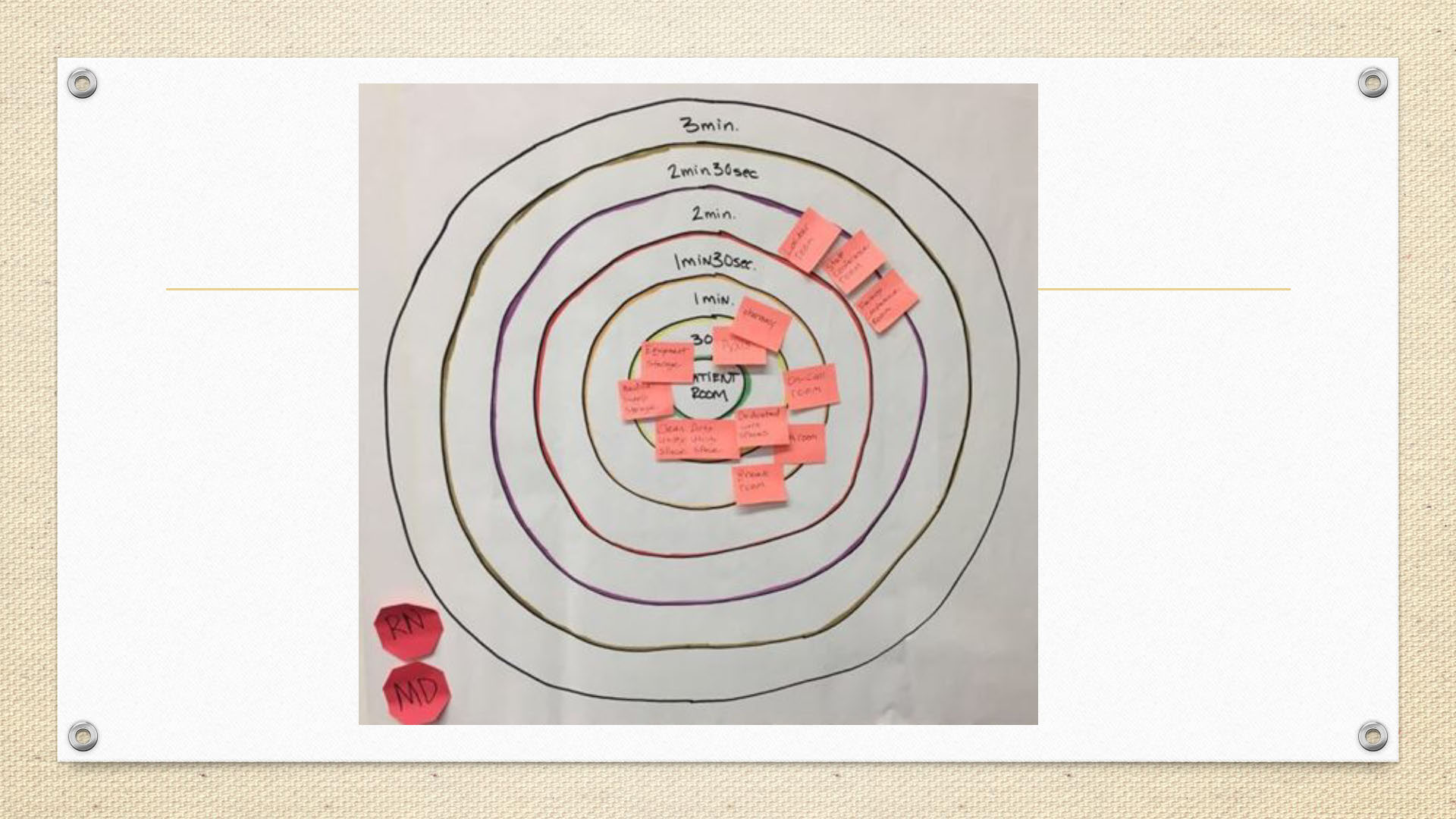
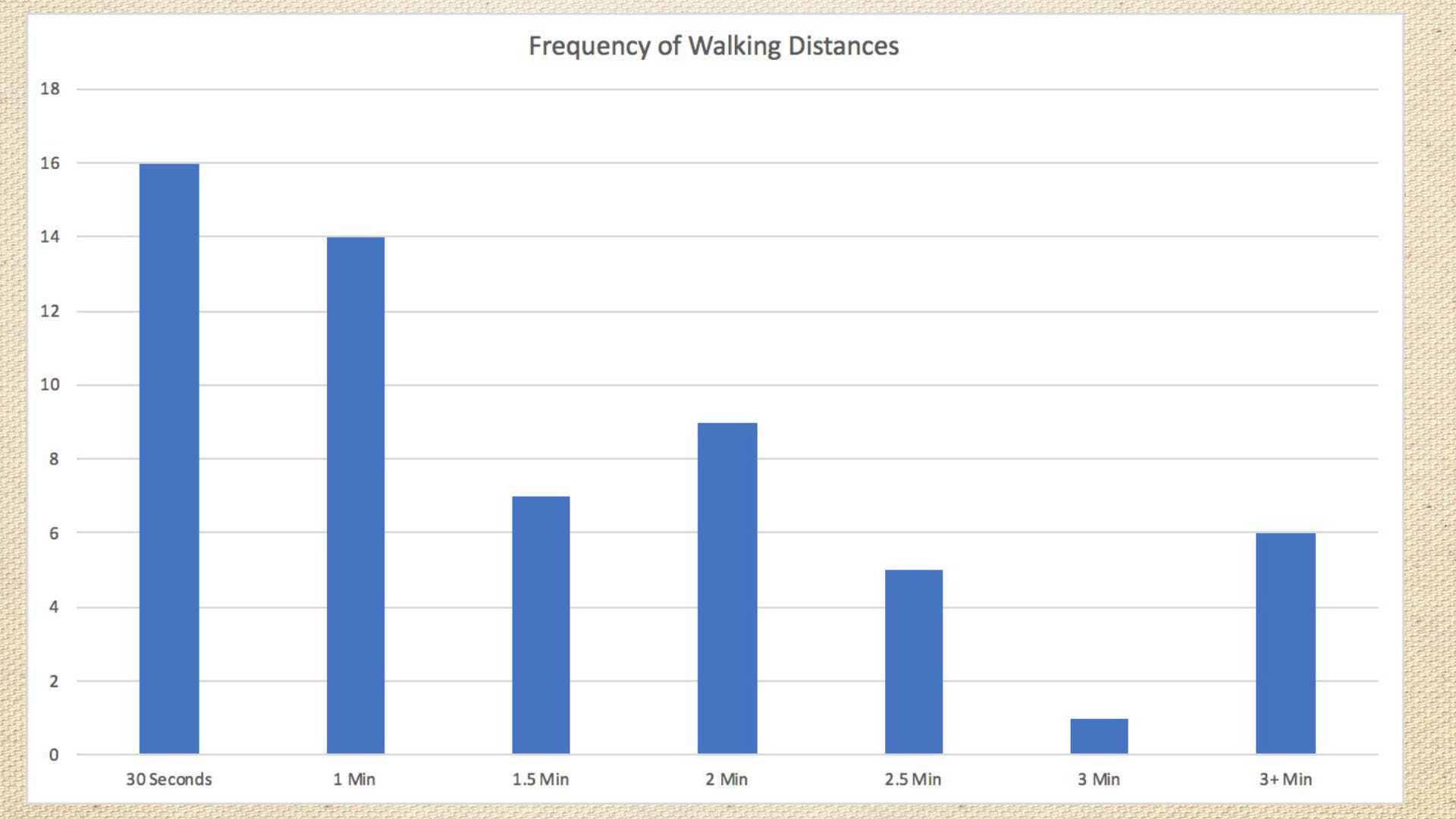
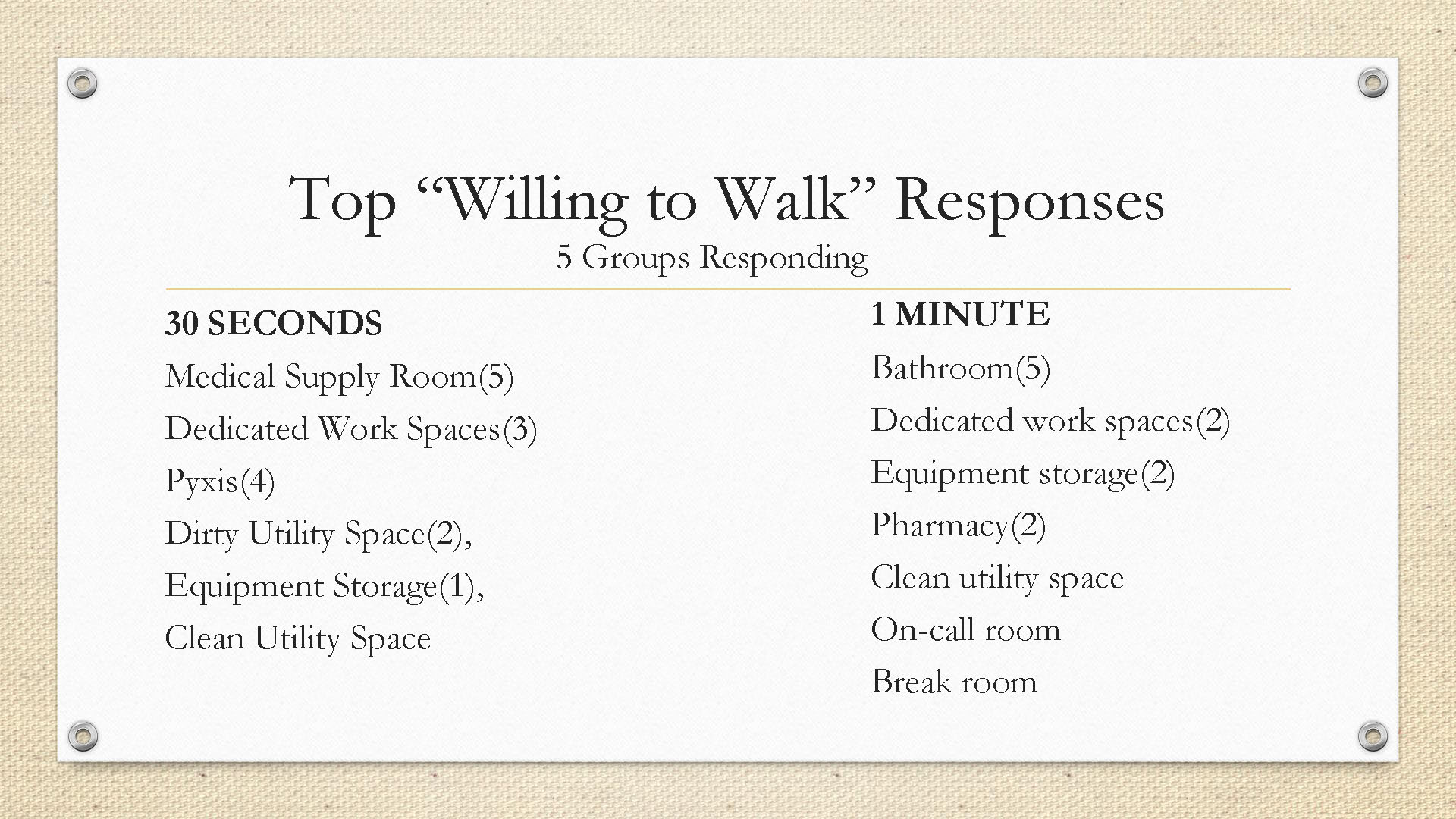
We created a generative session where we had the staff chart the ideal time one designated room/space needs to be from another. We charted these as concentric circles measured in units of time.
After the completion of this exercise, they were asked to pick out their most favorite and lease favorite rooms for each dedicated space so as to activate their thinking with regards to what they preferred and what they did not. These were also charted on Excel sheets for later analysis. This was later discussed with the rest of the class as a quick presentation so everyone is kept abreast of the progress in each of the groups (and sub-groups!). The process presentation:
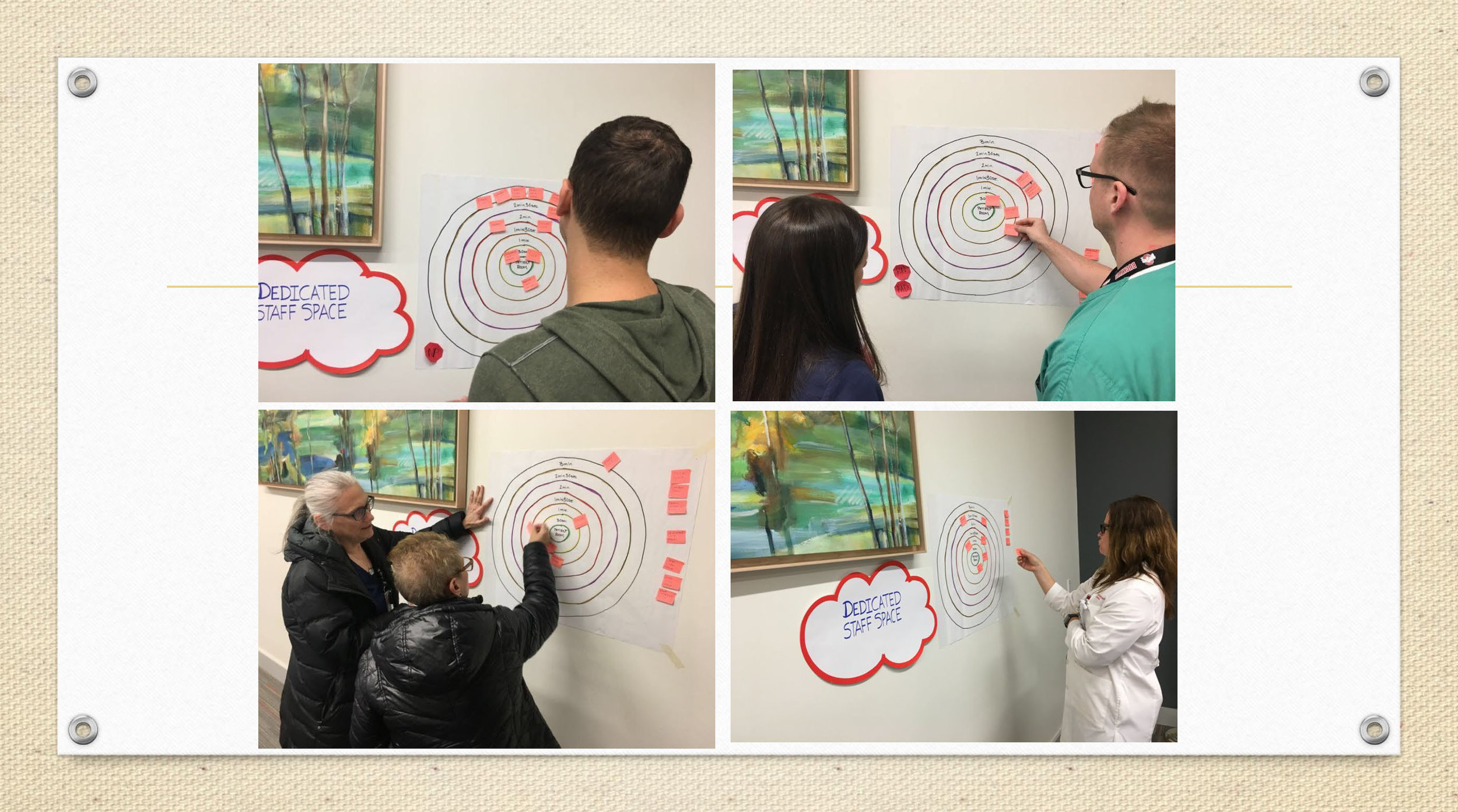



With each rotation of teams and workshops, we would reconvene and make sure the whole team of co-designers are informed about all facets of the research.
PHASE 3: ANALYSIS, FINDINGS, AND PROPOSALS
Here is a quick glimpse of the observations that came out of this co-design process:
We documented 255 observations from the touring, shadowing, and first workshop.
In Workshop 1, us co-designers identified 31 things that are working an 47 opportunities for improvement.
Based on the priorities of the co-designers, we narrowed the 47 opportunities down to the top 8.
We also generated a large number of preliminary ideas for the future (2030 and interim).
The Top 8 Observations from the Co-Design Process
Unit
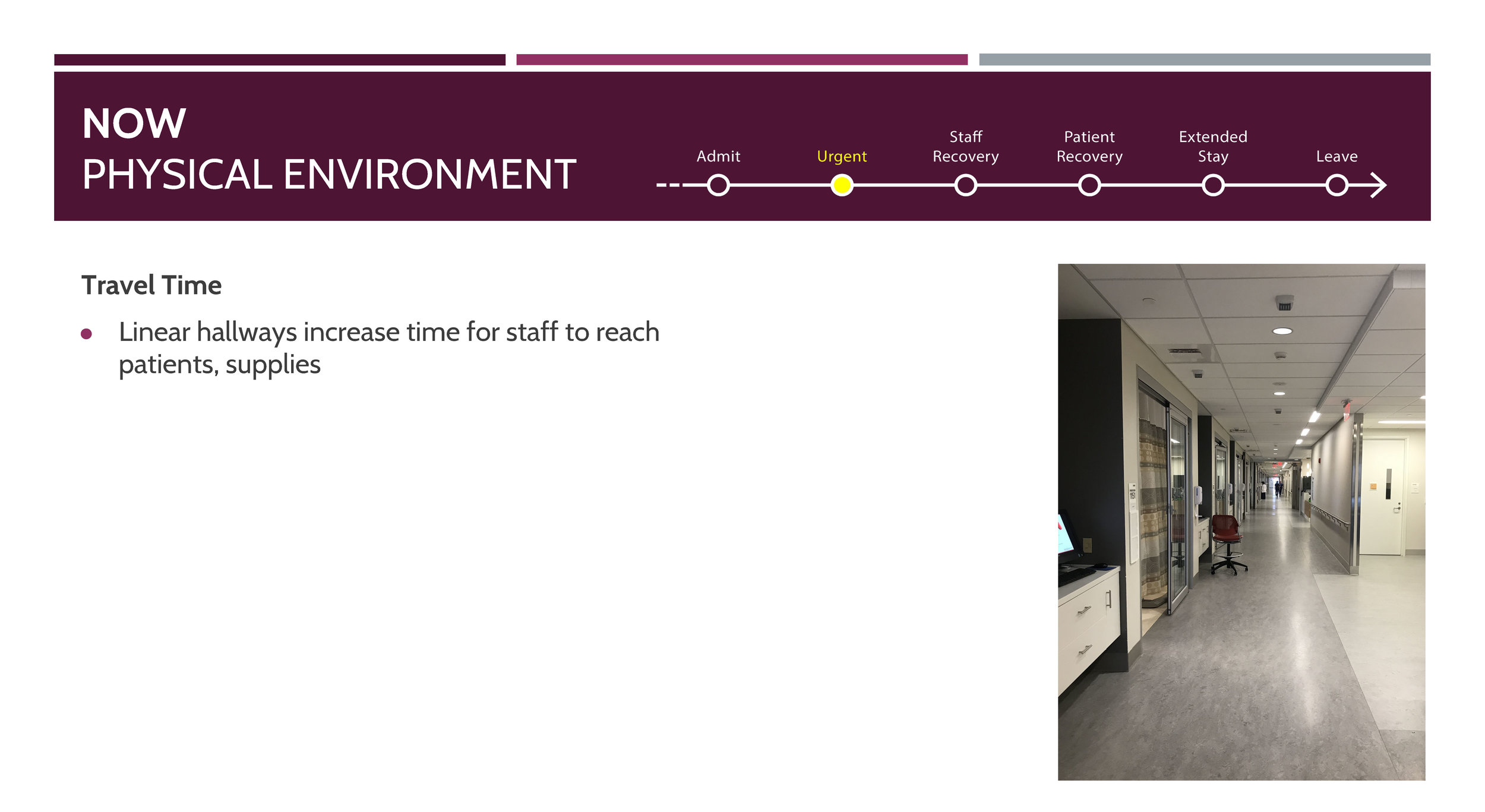
Linear vs. pod design for the layout
Dedicated spaces to meet the needs of the SICU staff
Room
Redesign of the sharps containers
Medical booms (Booms are used in healthcare facilities where there is a need for access to medical gases such as oxygen, nitrogen, and carbon dioxide, electrical power and audio-visual data services)
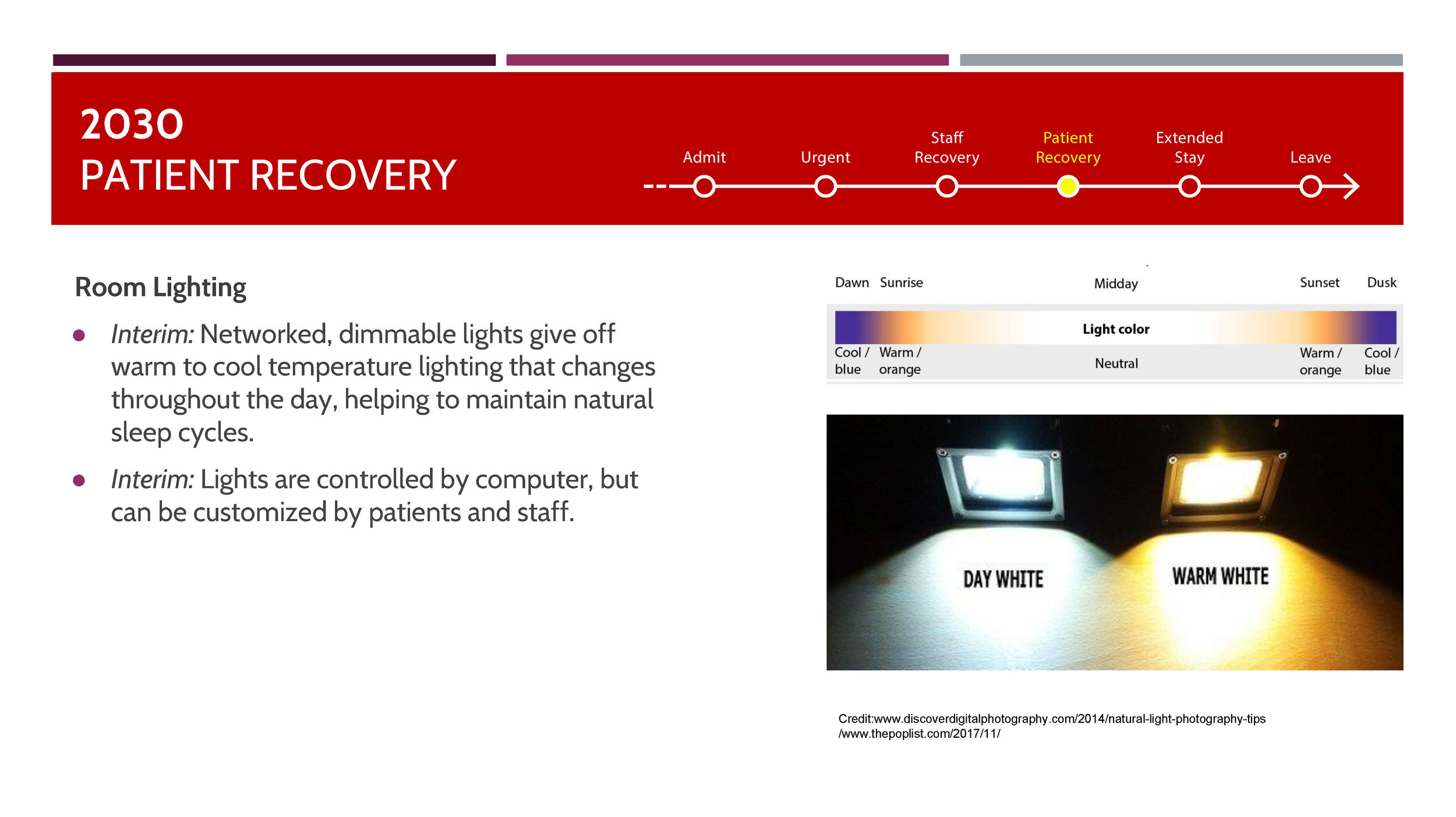
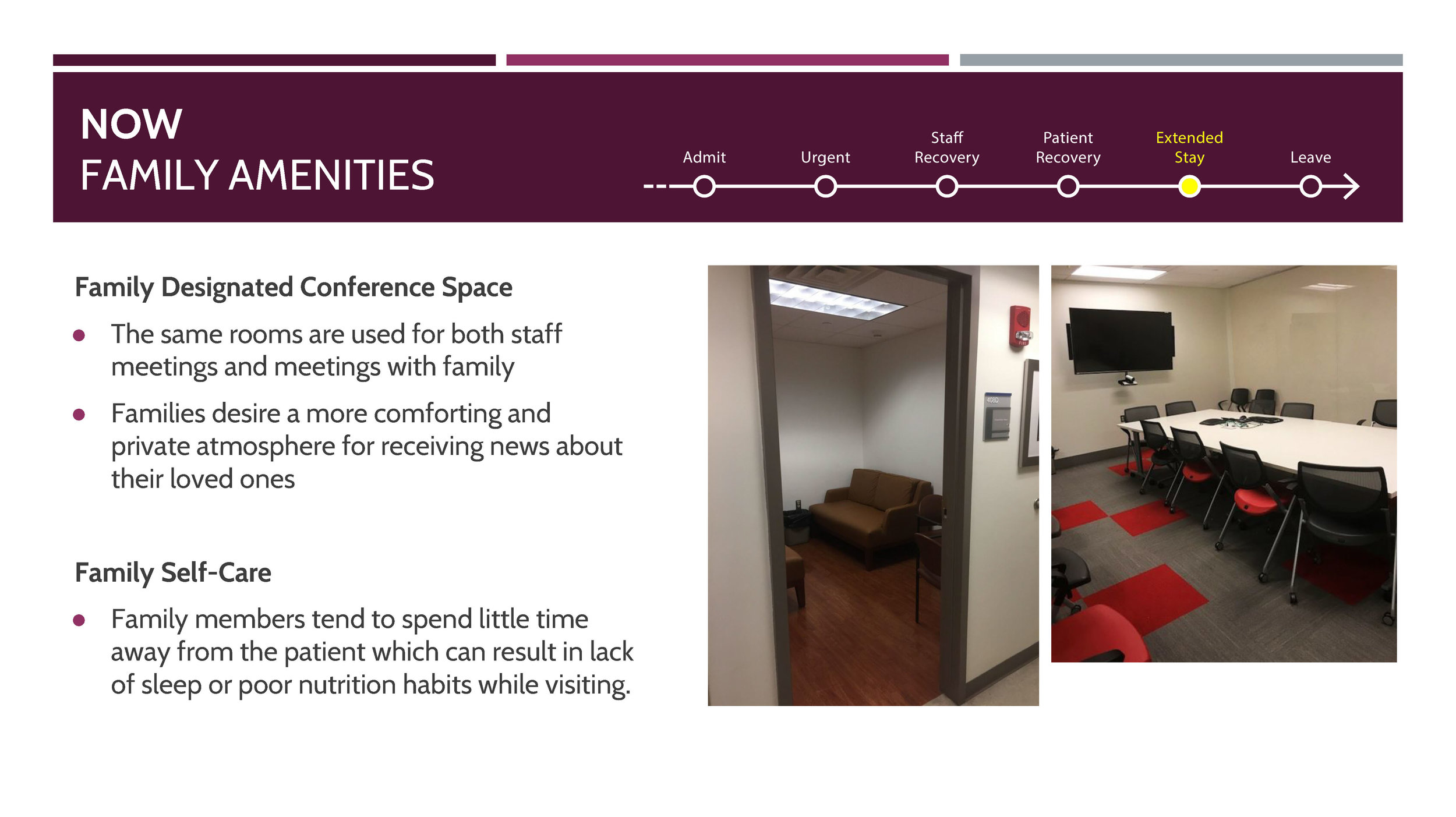
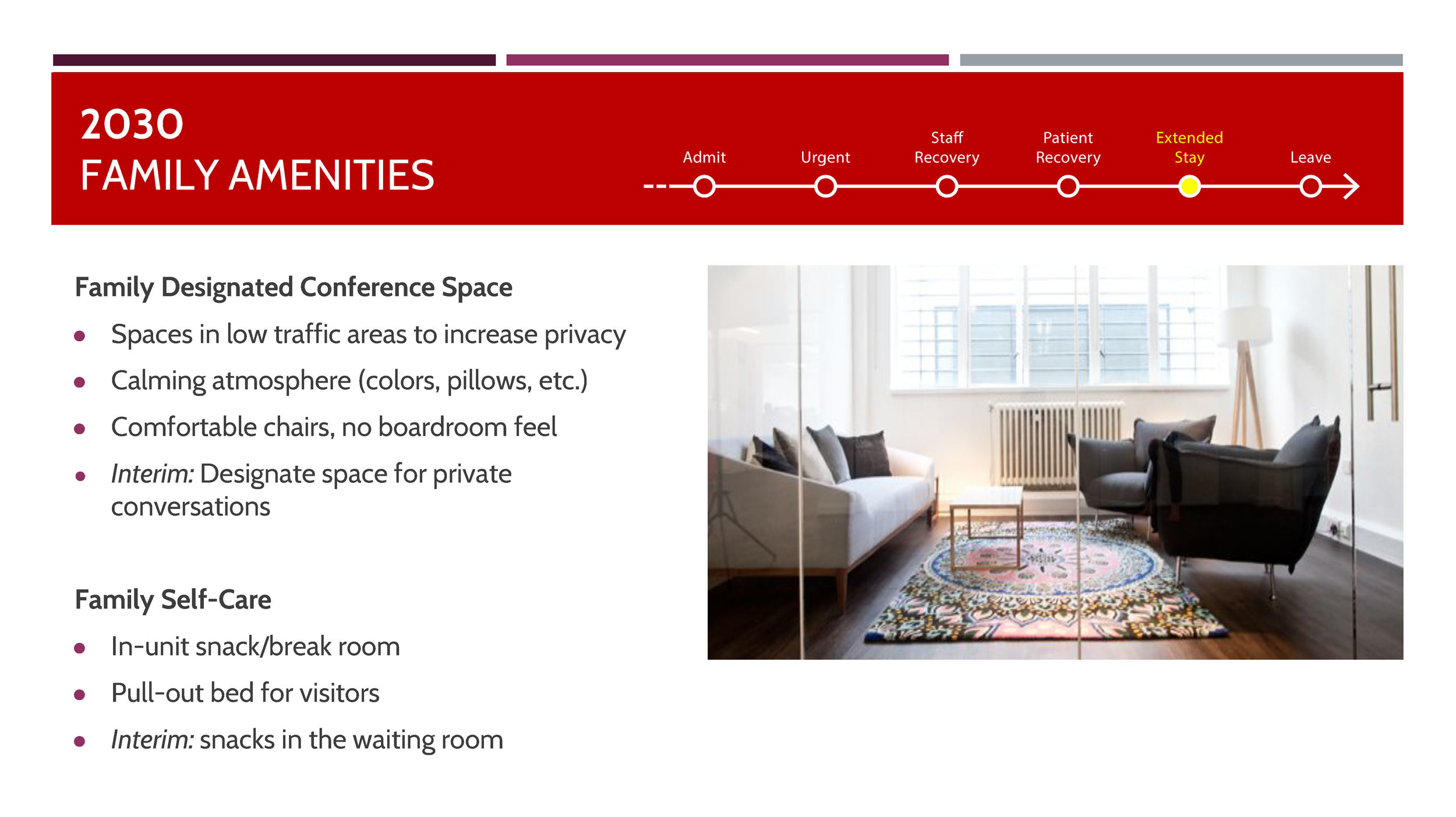
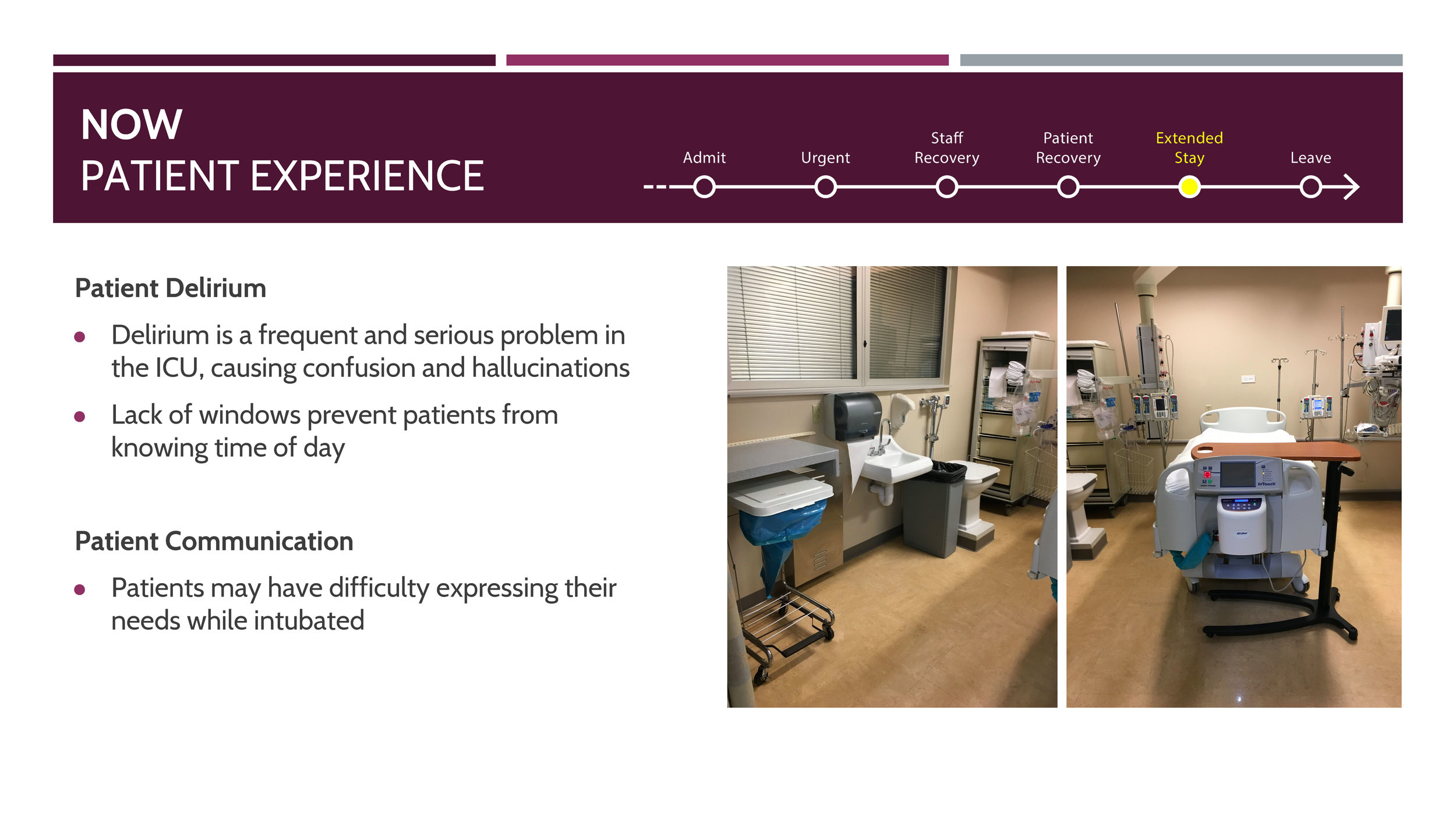
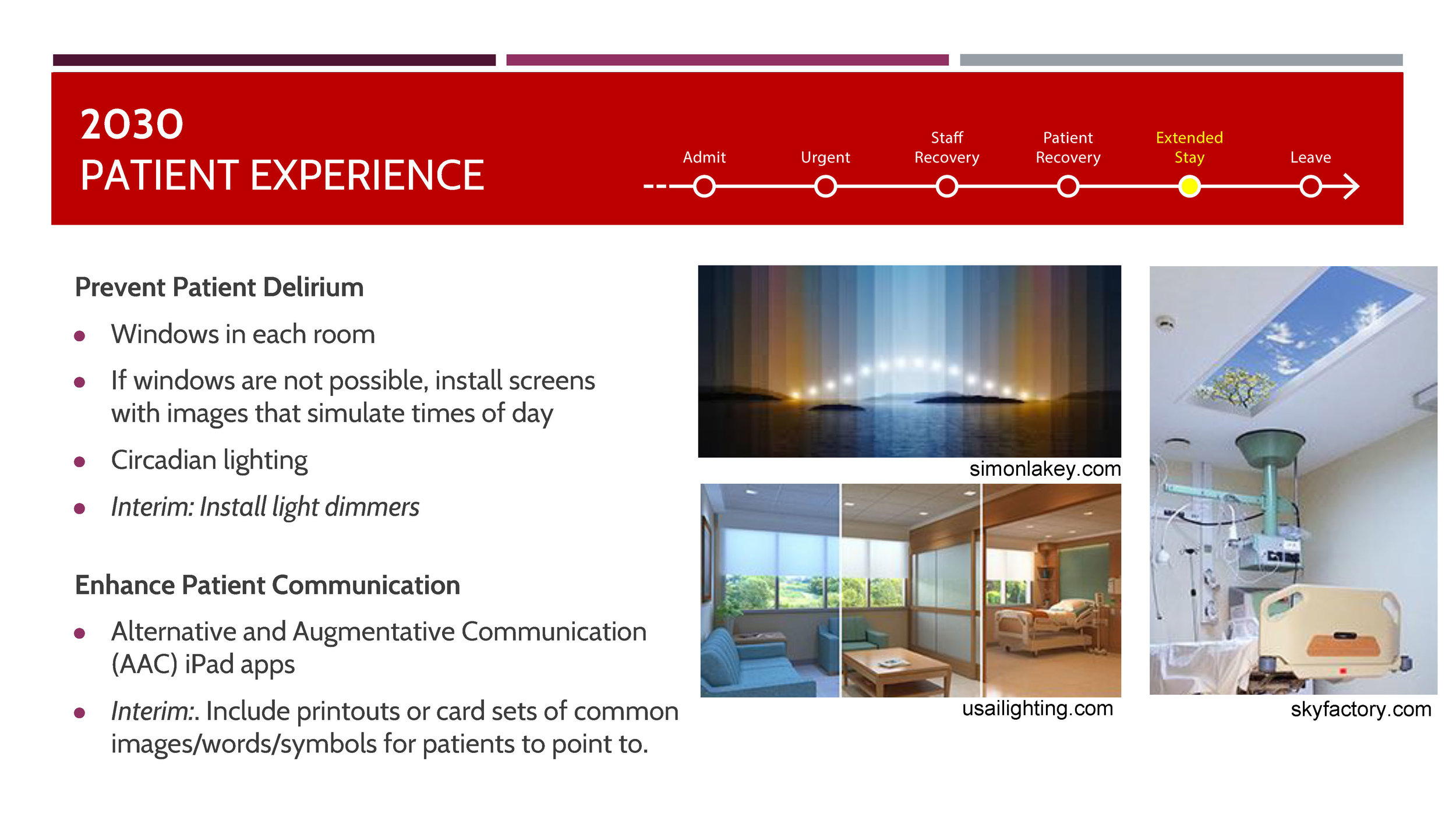
Lighting: Natural and artificial lighting from the perspectives of staff, family, and patients
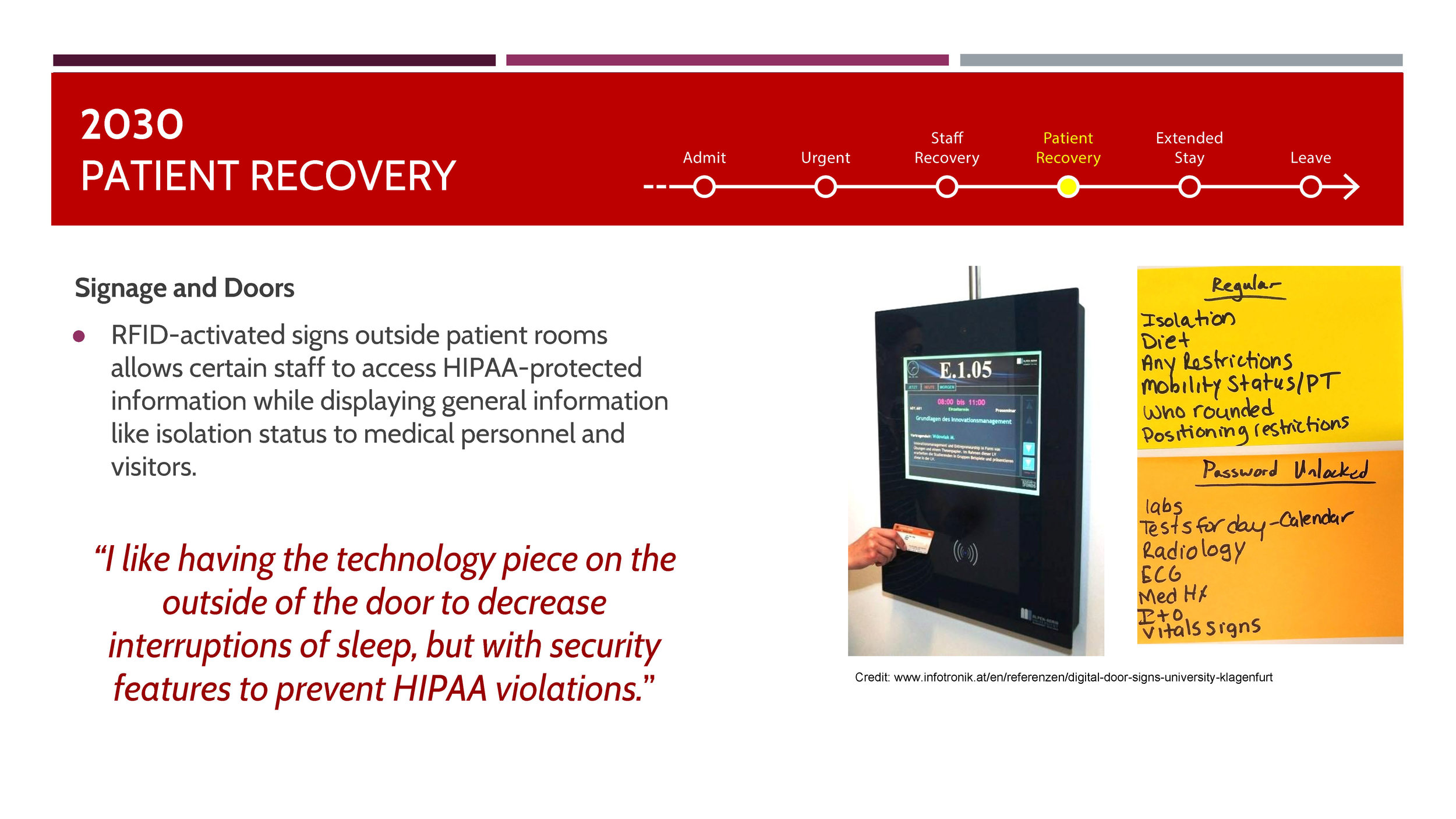
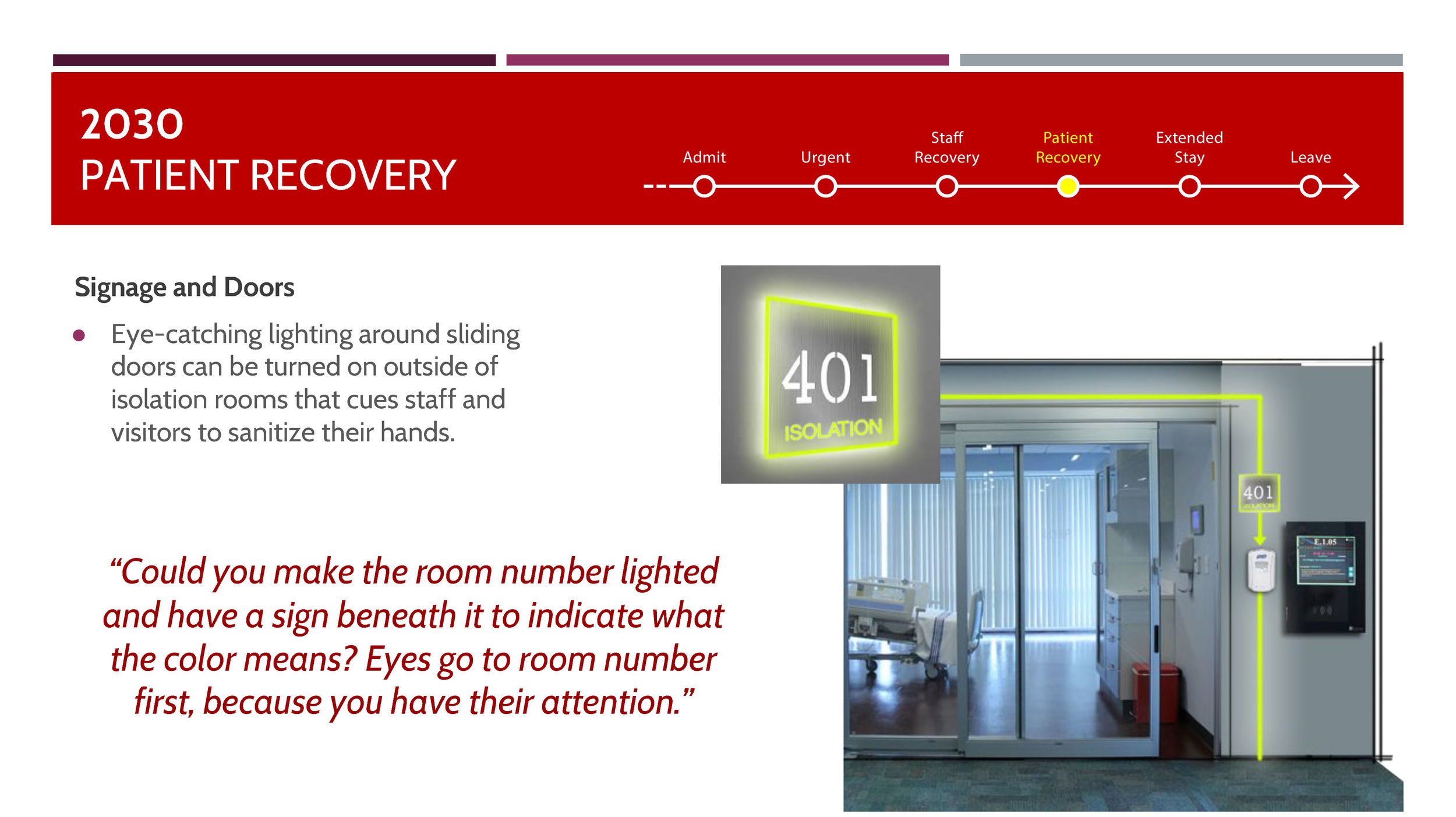
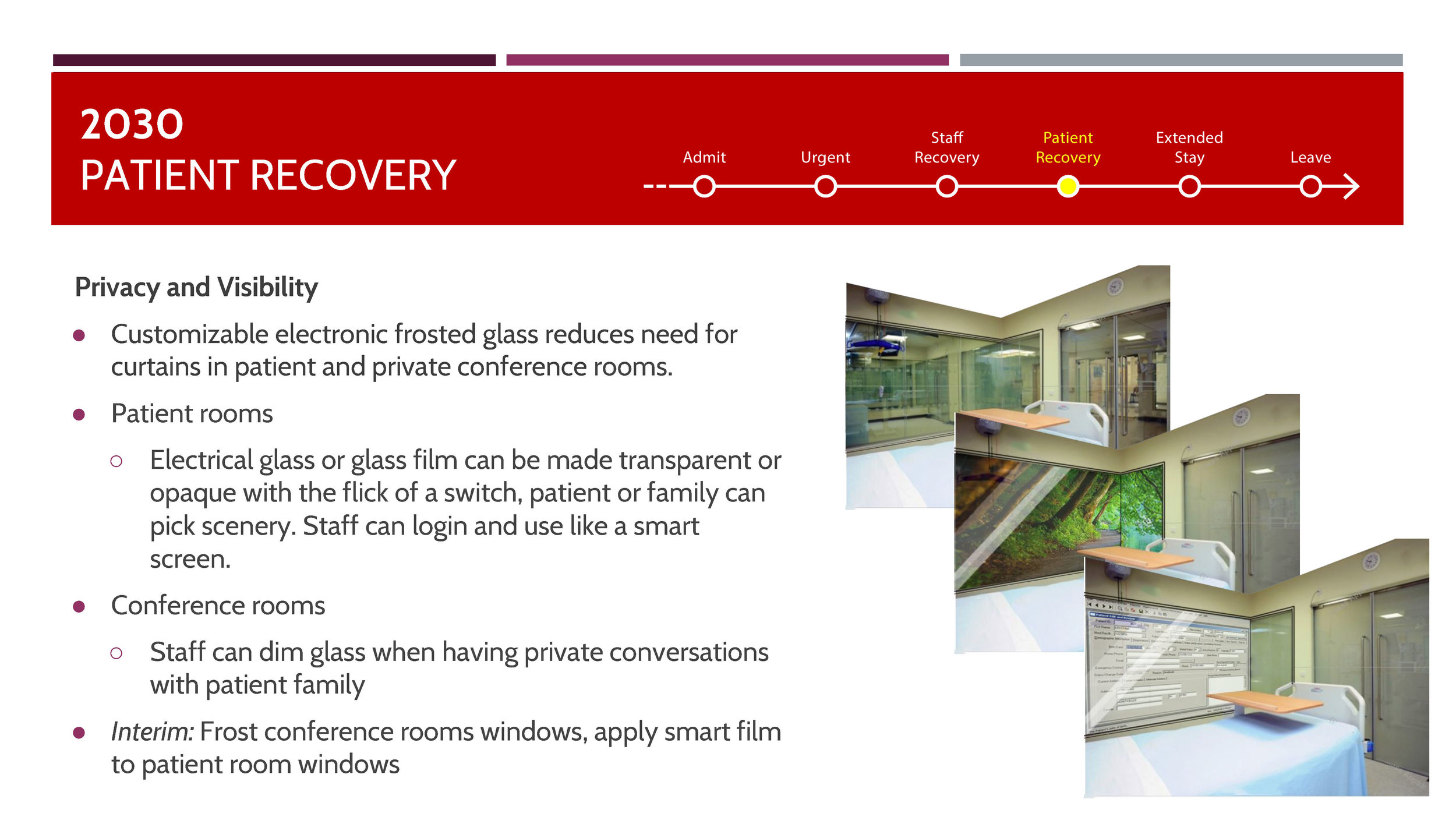
Visibility vs. Privacy of the patient/family from outside the room door
Experience
Communication b/w staff members as well as between staff and family
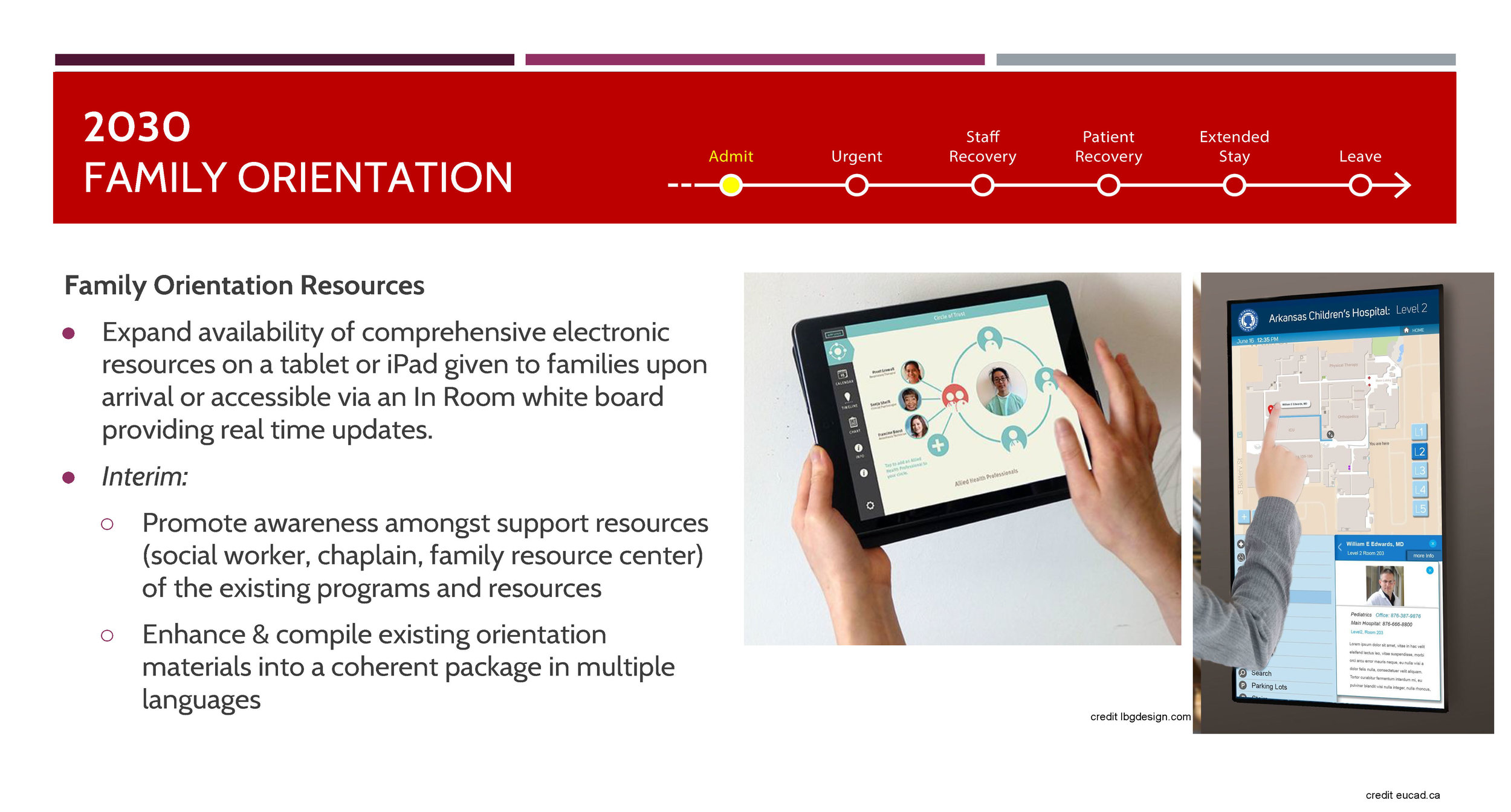
The patient/family SICU experience
The findings of this process was presented at the Surgical Innovations Symposium 2018 to an audience of medical professionals, medical infrastructure manufacturers, academics, etc. It was met with great intrigue and good reception and there is a possibility of us collaborating with the institution further.
For this presentation, we employed the use of a persona and a story to explain the main observations.



KEY LEARNINGS
To work with interdisciplinary teams, especially in the field of medicine and the kinds of constraints, rules and regulations as laid down by the medical board.
To not have a silo-ed approach or working but to quickly adapt to multiple phases and topics of research— we rotated teams almost every two weeks and that allowed us to get intimately acquainted with the whole project and not just one piece of it.
Time Management: It was really difficult to coordinate and have the doctors, NPs, nurses, RT/PT, etc., for the workshop sessions. With limited time, our sessions needed to be designed to make the most of it.
Immersion into secondary research: It was important not only to have literature on the subject but fully immerse ourselves in the space and situation to be able to start with a good footing of knowledge of how things are currently.
Generative Design research, as always, proved to be an effective tool. The medical staff mentioned toolkits being useful as a means to express their everyday activities (they might not think it is a big deal) that they might have skipped, had they just been talking about it.
Collaborative working- it definitely made me a much better team player.
Facilitation, organization, and detailed documentation methods and practices.